Hot New Therapeutic MOAs versus Neurodegenerative Diseases
By Wayne Koberstein, Executive Editor, Life Science Leader
Follow Me On Twitter @WayneKoberstein
Part one of three parts: Aiming at Alzheimer’s
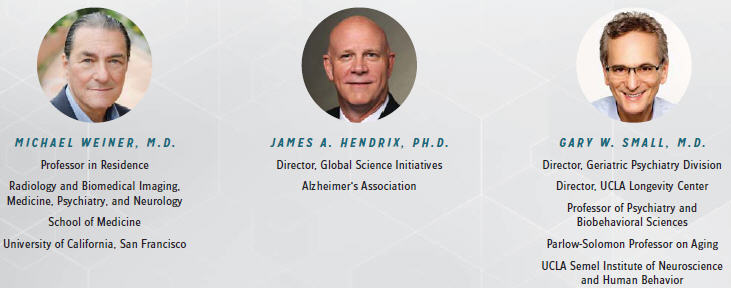
The following key opinion leaders (KOLs) participated in this “virtual roundtable” on new therapeutic approaches in development for Alzheimer’s disease.
This series is our second “deep-dive” into a hot new therapeutic area, the first being “Combination Cancer Immunotherapy — A Virtual Roundtable.” (September 2014 to January 2015, with a September 2015 update.) Here we dive into the neurodegenerative diseases (NDs) area — where a long, dark period of disappointment and frustration may be giving way at last to a flush of new therapeutic approaches based on previously unidentified or poorly understood mechanisms of action (MOAs).
Our virtual roundtable stitches together the separate inputs of participants into one comprehensive discussion, capturing the key players and issues at the dawn of revolutionary new modes of treatment. It brings together a panel of disease experts — key opinion leaders and scientists who are leading some of the most advanced research in the ND field. For comparison, and a closer look at the business side of the awakening ND space, we also cameo some of the companies in various stages of developing original agents that employ new MOAs.
Recognizing the considerable overlap of disease mechanisms and treatment issues among the many NDs, this series concentrates on the three most prevalent and representative of them: Here, Part One covers Alzheimer’s disease (AD). In subsequent months, Part Two will explore Parkinson’s disease, and Part Three, multiple sclerosis and other NDs.
Our limited sample of companies involved in the space suggests the range and variety of new MOA and drug development therein. (See the sidebar “Alzheimer’s Advances — Development During Debate,” and the table “New Therapeutic MOAs: Alzheimer’s Disease.”) Similarly, the small but prestigious panel of KOLs represents a range of leading views.
Our virtual panel discusses not only the scientific, regulatory, and other practical hurdles that lie before the new approaches, but also the issues that will affect any candidates that ultimately survive the development gauntlet and enter medical practice. Those include the possible use of therapeutic agents with different MOAs in combination, as well as the methods and authority for configuring combinations, along with pricing, postmarket regulation, and patient education.
MIRACLE OR MIRAGE?
Our KOL panelists, Drs. James Hendrix of the Alzheimer’s Association, Gary Small of UCLA, and Michael Weiner of UCSF, begin by rating the chances and likely timelines of new MOA drugs in development for Alzheimer’s disease. Their views vary considerably, reflecting the ongoing debate in the field as a whole.
What are the most promising therapeutic targets/mechanisms for Alzheimer’s?
HENDRIX: The most excitement in the Alzheimer’s field during the past year has been driven by the amyloid space. What made it exciting is the incorporation of amyloid imaging into some clinical trials, along with other amyloid biomarkers, such as CSF (cerebrospinal fluid). Those tools allow our clinical researchers to identify people with high levels of amyloid in their brain, so they can give an experimental drug to people who should respond to it — and that’s new.
WEINER: I’m a mainstream Alzheimer’s scientist, and I see the disease as closely associated with two misfolded proteins, amyloid beta and tau. By definition, to have Alzheimer’s disease, you must have both proteins. Although not proven yet, there is a huge amount of evidence those proteins are the causes of neurodegeneration. The problem with developing a treatment aimed at general mechanisms such as neurodegeneration is that they are tied to the normal machinery of the cell. The more specific the target and the more specific the treatment, the less chance there is for side effects. That’s what the industry is doing with passive immunotherapy, the monoclonal antibody (mAb) amyloid blockers such as solanezumab and aducanumab.
As people age, one reason they accumulate misfolded proteins is immunosenescence — the immune system ages to the point where it can no longer generate a strong antibody response to those proteins. How can we ramp up the immune system to respond better to these diseases? That’s a long-term question. Meanwhile, we would like to see more efforts directed at preventing the formation of phosphorylated tau tangles, which is more closely associated with synapse loss and neurodegeneration than amyloid plaque.
SMALL: There are a lot of mechanisms in the brain besides amyloid and tau. In Alzheimer’s disease, there’s also evidence of inflammation. Despite the tremendous focus on antiplaque, so far it has not panned out. Even though we see a mechanism, we are not quite sure how to disrupt that mechanism to benefit the brain. Some of the changes we see may be just a result of some other neuropathic states underlying those mechanisms. I am a big advocate of diversifying our research portfolio, because we are not sure what will score a hit. In some of the clinical trials with anti-inflammatory treatments, there seems to be a benefit if used early, but exacerbation if used later.
HENDRIX: The biomarker studies, particularly the collaborative Alzheimer’s disease Neuroimaging Initiative (ADNI) study, have shown that changes occur in people’s brains as much as 10 years before cognitive symptoms occur. If we can identify those people early and prevent the disease progression, we could have much better outcomes. Our hope is we’ll eventually be able to delay the onset of the disease for a long enough period that people will live long enough to die of a different disease, and with their memories intact.
COCKTAIL CALL?
No one seems to argue for monotherapy in Alzheimer’s disease, though the KOLs may disagree by degree about the therapeutic bandwidth of potential “cocktail” regimens. With so many non-exclusive targets in the long, complicated disease pathway, combination therapy for Alzheimer’s seems inevitable.
How likely is it that some future drug therapies, each one hitting a different target, will prove complementary if used together? Could combination drug therapy then become the paradigm for treating a disease such as Alzheimer’s?
SMALL: If I had to choose between a highly effective symptomatic treatment for Alzheimer’s, taken for the duration of the illness, versus a disease modifier such as an amyloid blocker, where it takes longer for any modest benefits to kick in and side effects can be significant, I might choose symptomatic. But if I were free to prescribe both kinds of treatment, I would, because I want to do whatever I can to keep someone’s brain healthy. So we may see a new form of polypharmacy emerging in this space.
HENDRIX: An Alzheimer’s Association workshop in April 2015 brought together experts from pharma, government agencies such as the FDA and NIH, and academia to address the issue of combinations. The general feeling was the amyloid approach may provide some benefit, but the maximum benefit may come when you combine at least two different mechanisms such as amyloid and tau, and that could be the standard approach in the future.
Besides the disease-modifying drugs, there are also symptomatic therapies in the pipeline combining different mechanisms of action, such as 5-HT6 antagonists in combination with the already approved cholinesterase inhibitor, donepezil. A recently approved combination therapy, Namzaric, is donepezil with the NMDA-blocker memantine [Namenda]. But those drugs become less and less effective as the disease progresses, so we still need therapies that slow progression. A third type of drug in clinical trials addresses psychiatric symptoms of the disease. We need all of those approaches to treat the disease as a whole.
Could combinations of new drugs pose medical, regulatory, or economic issues for treatment of Alzheimer’s?
HENDRIX: The most important issue from a regulatory approach is, if you’re testing a drug in combination, does it need to be synergistic, or can it just be additive? To date, the regulators have indicated an additive effect is good enough, but safety is an issue with any drug in a combination — for example, avoiding a harmful drug-drug interaction. Of course, there is the issue of cost, and some drugs can be quite expensive, particularly the biologicals. But we know Alzheimer’s disease is hugely expensive today and will be much more so in the future, so a combination drug therapy, though expensive, may still be a bargain compared to having no effective treatments.
SMALL: Companies are naturally concerned about how much payers will support how their products may be used or combined. A treatment algorithm will eventually evolve based on the data and determine access to any particular drug or set of drugs. But I doubt the companies or NIH grantees will be able to study that decision-making process systematically. Even in the medical community, I suspect reaching a consensus on the criteria will be a bit of a struggle.
FOR INDUSTRY: DUTY & DIRECTION
The panel offers a variety of advice for how companies and the industry as a whole can speed the advancement of new therapies for Alzheimer’s.
What does the pharma/biopharma industry need to do to ensure the new treatments reach patients, and soon?
WEINER: Companies must do successful clinical trials and get the treatments approved by the regulators, but the biggest single obstacle is recruitment of patients into the trials. Trials in this field enroll slowly and have high dropout rates because it’s hard to get patients to continue, especially at early stages of the disease when we’re after subjects who are not seeking treatment. To help solve the conundrum, we started The Brain Health Registry, thebrainhealthregistry. org, where we encourage people to sign up, take some tests, and answer some questions, and then we refer them into clinical trials. We already have 35,000 people enrolled. We believe this new Web-based approach will help accelerate clinical trails in this area.
HENDRIX: The drug development and the drug approval expertise in this country, and in the world, resides in the pharmaceutical industry. If we don’t motivate companies and keep them interested in doing Alzheimer’s R&D, we all lose. The whole ecosystem of research must be strong, from academia, to government, to the private sector as well, along with support from nonprofit organizations such as the Alzheimer’s Association.
We need to continue to pressure our political leaders to provide more research funding because our researchers need help. The other advice I have for people in the industry is to make sure that you are an advocate for Alzheimer’s treatment in your own community. Everyone in the United States can now have a “wellness” visit with a doctor, and if you’re in Medicare, you can have a cognitive assessment done to check your brain health. Everyone needs to do that — physicians need to insist on it, and patients need to insist on it. We must distinguish between normal aging and disease.
A BROADER MOA AGENDA
Perhaps the efforts of researchers and developers in the Alzheimer’s area will also contribute to progress in others, and vice versa.
To what extent might the underlying causes for multiple neurodegenerative diseases (NDs) be similar or the same — and thus perhaps respond to the same therapeutic MOAs?
SMALL: The brain is a very complex organ, and these diseases are also complex; many different neurotransmitter systems and brain abnormalities are involved, so there’s tremendous overlap. Take the first drugs that were developed to treat the symptoms of Alzheimer’s, the cholinesterase inhibitors. The cholinergic neurons are important for normal brain function, in general. Even though the indication for those drugs is primarily for Alzheimer’s dementia, they still benefit some of the other conditions: Lewy body dementia, Parkinson’s dementia, and so forth.
WEINER: There is a large class of neurodegenerative diseases that all appear to be associated with misfolded proteins: Alzheimer’s disease, which is associated with amyloid beta and tau; frontotemporal dementia, with tau and other proteins; Lewy body disease and Parkinson’s disease, with alpha-synuclein; amyotrophic lateral sclerosis, with SOD1 [superoxide dismutase 1] or TDP-43 [TAR DNA binding protein]; and a number of other neurodegenerative diseases. But the proteins involved in each disease are quite different. Neurodegeneration is the ultimate common pathway for a lot of diseases, so some laboratories have aimed at trying to block apoptosis or other neurodegenerative processes, but the majority of the field is aimed at specific proteins.
HENDRIX: The Alzheimer’s Association has partnered with the Michael J. Fox Foundation, Alzheimer’s Research UK, and the Weston Brain Institute in Canada, on grant opportunities for researchers looking at where the causes of different NDs could overlap, as in neuro-inflammation. If Parkinson’s and Alzheimer’s both involve misfolded proteins, do the proteins normally misfold but start accumulating instead of being cleared out of the brain as usual? If we understood that basic molecular question, we would have a better way to attack these diseases, including the orphan diseases that share the same effect. There has been some research about a hypothetical clearance mechanism, but we don’t know whether the basic problem is clearance or inflammation.
What other issues or challenges in developing new drugs and MOAs for Alzheimer’s disease concern you?
HENDRIX: Of the top 10 causes of death in the United States, Alzheimer’s is the only one for which no way exists to stop or slow the disease, and even though we’ve recently seen additional funding of $350 million from the federal government for the NIH, we still don’t fund Alzheimer’s research at the levels of cancer, for example. In 2014, a blue ribbon panel convened by the Alzheimer’s Association concluded we would need $2 billion a year in research funding from the NIH for the next 10 years to reach the national goal of an effective treatment or cure for Alzheimer’s disease by 2025. We spend $226 billion per year on care for the disease right now; without therapeutic progress, care costs will balloon to $1.1 trillion by the middle of the century.
Alzheimer’s disease funding had been stuck at just under $600 million per year, but even in this very partisan time, and with tremendous rancor in D.C., this year we convinced both sides of the aisle that Alzheimer’s needs additional funding, so the funding is now nearly double of what it was just a few years ago, for which we are very grateful. But it’s still not $2 billion a year. We have much more to do.
SMALL: One of the simple facts that motivates me is that we don’t really have that much to offer Alzheimer’s patients yet. It is frustrating and tragic and family members feel helplessness when they realize the doctors can do nothing more to help them. But I believe in time we can. It’s a question of us being smart and pursuing a strategy that will be successful. It is not just about getting more candidates into your clinical trials, but also about being objective and meticulous in focusing on what makes sense in getting the right data.
Another area where improvement could help drug development is the interface between academia and the pharmaceutical industry. It can be awkward for academics, as they say in the industry, to go from bench to bedside, and I know our university and others have been working on how to make it easier. Although there are many intelligent and gifted investigators in our universities, they are not typically trained in how to make that journey, how to take their research to the next level. Basically, in academia, we are taught to publish or perish, not publish or produce.
WEINER: We need a whole big public awareness campaign — a big media, public relations campaign. We must get older people to start realizing Alzheimer’s disease is a common problem, Alzheimer’s disease runs in families, Alzheimer’s begins with mild memory problems, and the only way we will see new treatments is for people to participate in clinical trials. Each time the FDA approves a new, effective treatment for the disease, there should be massive campaigns to get those treatments into practice, and the market will take care of that.
Please look for Part Two of this series next month, focusing on new therapeutic MOAs for Parkinson’s disease.
ACCERA
Enrolling a Phase 3 trial of its ketone-based glucosemetabolic substitute.
Charles Stacey, President and CEO: During the past 10 years, the failure rate for Alzheimer’s drugs in Phase 2 and Phase 3 has been 99.6 percent, which is higher than for any other indication. One of the main reasons is the industry as a whole is really focused on the amyloid hypothesis, but whether the hypothesis explains a cause or effect has really never been established. We need to have more mechanisms of action. We need to diversify the targets we’re looking at. As a company, we are addressing a different mechanism with our lead compound, AC-1204. It is well known that in Alzheimer’s disease there is a metabolic deficiency within the brain — the brain becomes starved of its fuel, glucose, and goes into a neurotoxic decline, and the neurotoxicity leads to cell death. Our drug replaces glucose with ketone bodies that can serve as an alternative fuel to reverse the neurotoxic cascade.
NEUROGENETIC PHARMACEUTICALS
Completed positive preclinical PoC (proof of concept) clinical safety study for a small molecule drug that modulates the gamma secretase complex in amyloid-plaque production to suppress toxic plaque.
 William T. Comer, Ph.D., CEO and Chairman: You can’t treat people with advanced Alzheimer’s; it’s too late. You can’t cure a dead brain. You’ve got to prevent the disease, but how? You must go back in the system and see what causes the problem in the first place. We believe it’s the toxic form of amyloid plaque, but the first amyloid antibodies failed in trials — because the FDA limited them to patients who were too far advanced. But the anti-amyloid strategy appears to work when it targets an earlier population. It’s well understood that cognitive impairment probably occurs years after amyloid deposition begins. Thus, if you use cognitive impairment as your early diagnostic, the amyloid and tau pathologies are already too advanced to reverse or prevent Alzheimer’s disease.
William T. Comer, Ph.D., CEO and Chairman: You can’t treat people with advanced Alzheimer’s; it’s too late. You can’t cure a dead brain. You’ve got to prevent the disease, but how? You must go back in the system and see what causes the problem in the first place. We believe it’s the toxic form of amyloid plaque, but the first amyloid antibodies failed in trials — because the FDA limited them to patients who were too far advanced. But the anti-amyloid strategy appears to work when it targets an earlier population. It’s well understood that cognitive impairment probably occurs years after amyloid deposition begins. Thus, if you use cognitive impairment as your early diagnostic, the amyloid and tau pathologies are already too advanced to reverse or prevent Alzheimer’s disease.
We should treat patients when we can prevent significant cognitive impairment by reducing the amyloid plaque so the condition doesn’t get worse. Our company has a novel and maybe more effective way of addressing toxic plaque early. Our gamma secretase modulators (GSMs) are based on an innovative modulation of a key enzyme in the amyloid pathway, called γ-secretase. The approach with our lead product NGP 555 is to alter the production of amyloid proteins from the toxic form found in AD brains (Aß42) to nontoxic forms (Aß37 and Aß38), which do not contribute to plaque deposition.
NEUROPHAGE
Positive preclinical PoC studies for its general amyloid interaction motif (GAIM)- based drug for neutralizing misfolded proteins such as toxic amyloid plaque.
 Richard Fisher, Ph.D., Chief Scientific Officer: The basic cause of Alzheimer’s and other neurodegenerative diseases is toxic, misfolded proteins. Part of the toxicity of misfolded proteins in the brain comes from their aggregation. A misfolded protein ends up in a conformation that allows it to aggregate to other misfolded proteins of its kind and those eventually end up along a pathway to becoming oligomers, which are a relatively small number of subunits of the misfolded proteins stuck together. Those aggregates are very toxic and, in the brain, very toxic to neurons. The pathway can continue all the way to a fiber, so it’s a large aggregate, a big polymer, and then the fibers can also stick together and they make extracellular plaque in Alzheimer’s called A-amyloid plaque, and they can go on a similar pathway with tau, ending with neurofibrillary tangles. In Parkinson’s disease, alpha-synuclein ends up being a misfolded protein that assembles along the pathway into aggregates that become fibers that stick together and form Lewy bodies in the brain — especially in the substantia nigra, the part of the brain involved in motor function.
Richard Fisher, Ph.D., Chief Scientific Officer: The basic cause of Alzheimer’s and other neurodegenerative diseases is toxic, misfolded proteins. Part of the toxicity of misfolded proteins in the brain comes from their aggregation. A misfolded protein ends up in a conformation that allows it to aggregate to other misfolded proteins of its kind and those eventually end up along a pathway to becoming oligomers, which are a relatively small number of subunits of the misfolded proteins stuck together. Those aggregates are very toxic and, in the brain, very toxic to neurons. The pathway can continue all the way to a fiber, so it’s a large aggregate, a big polymer, and then the fibers can also stick together and they make extracellular plaque in Alzheimer’s called A-amyloid plaque, and they can go on a similar pathway with tau, ending with neurofibrillary tangles. In Parkinson’s disease, alpha-synuclein ends up being a misfolded protein that assembles along the pathway into aggregates that become fibers that stick together and form Lewy bodies in the brain — especially in the substantia nigra, the part of the brain involved in motor function.
Misfolded proteins are sticky; they have sticky edges, unlike normally folded proteins, and they can spread through the brain no matter where they start, like a prion in Mad Cow or similar diseases. A misfolded protein causes properly folded proteins to misfold as well, acting as a template. That seems to be a general principle, even in misfolded proteins such as Abeta in Alzheimer’s, alpha-synuclein in Parkinson’s, and tau in Alzheimer’s and other tauopathies. And it is probably going on in some peripheral amyloidosis outside the brain.
Our drug candidate, NPT088, leads to the elimination of misfolded proteins eventually in the mouse brain or in tissue, but if you look at it biochemically, first there’s binding and then what we call remodeling of the structure, so essentially, the toxicity is neutralized. Our drug is a protein derived from a bacteriophage, a part of the virus that helps it enter bacteria cells. It has a shape that recognizes those misfolded proteins as they assemble.
COGRx (COGNITION THERAPEUTICS)
Going after various forms of protein misfolding and aggregation in multiple diseases, with its lead small molecule blocker of toxic beta amyloid in Phase 1 for Alzheimer’s.
Hank Safferstein, Ph.D., CEO: Our discovery and development program has delivered first-in-class receptor antagonists against the toxic forms of the Abeta protein. The company’s novel biological and chemical platforms have been the driving force behind the discovery of first-in-class therapeutics and their novel mechanism of blocking the binding and signaling of soluble Abeta oligomers. Among those are first-in-class small molecules that directly target toxic Abeta oligomer proteins and their receptors and stop their bad effects on memory, with demonstrated dose-dependent knockdown in toxic Abeta binding. We have also identified a new epitope on a known membrane-bound protein to which our drugs bind and can block or displace bound oligomers. Our Phase 1a clinical studies are under way, having completed the single ascending dose and first cohort from the multiple ascending dose study. All data generated to date indicates we have a wide margin of safety going into our Phase 2 study in Alzheimer’s patients.
TETRA DISCOVERY PARTNERS
This company, like many others, is an enterprise founded as the sole champion of a new therapeutic mode of action for Alzheimer’s and other neurodegenerative diseases — PDE4 inhibition.
 Mark Gurney, Ph.D., Chairman and CEO: Our drug in Phase 1 development, BPN14770, modulates a biochemical mechanism of memory fundamental to the human brain, PDE4D [phosphodiesterase 4], to enhance cell signaling between neurons in the brain, while maintaining information flow through brain circuits important for memory. BPN14770 does not address a specific neurochemical deficit or disease pathway, so we believe it will have broad cognitive benefit across multiple neurologic and psychiatric illnesses.
Mark Gurney, Ph.D., Chairman and CEO: Our drug in Phase 1 development, BPN14770, modulates a biochemical mechanism of memory fundamental to the human brain, PDE4D [phosphodiesterase 4], to enhance cell signaling between neurons in the brain, while maintaining information flow through brain circuits important for memory. BPN14770 does not address a specific neurochemical deficit or disease pathway, so we believe it will have broad cognitive benefit across multiple neurologic and psychiatric illnesses.
The PDE4 target had fallen out of favor due to the perception that a well-known side effect, nausea, could not be prevented. It also has been difficult to develop compounds that are selective for one of the four PDE4 subtypes, each of which have potentially distinct therapeutic profiles, but only one of which, PDE4D, appears to be associated with emesis. Our team solved the crystal structures of the PDE4 regulatory domains and developed PDE4 subtype-selective inhibitors based on this new knowledge. Because the drug has little effect on PDE4D in the off-state, it has very good tolerability.
NEW THERAPEUTIC MOAs: ALZHEIMER’S DISEASE
A list of the numerous modes of action employed by drugs approved or in development for treating Alzheimer’s disease, along with their company affiliations. Unless other indications are listed, all development stages or phases refer to the Alzheimer’s indication.
DISEASE MODIFICATION/PREVENTION
Anti-Beta Amyloid (Abeta) Plaque
mAbs - (Passive immunotherapy)
- Lilly: LY2062430 (solanezumab). Phase 3
- Biogen: aducanumab. Phase 3 enrolling
- Janssen, Pfizer: bapineuzumab. Phase 3 discontinued
Selective beta secretase (BACE1) inhibitors
- Merck: MK-8931 (verubecestat), Phase 2/3
- AstraZeneca/Lilly: AZD3293. Phase 2
Gamma-Secretase Modulators (GSMs)
- Anavex: ANAVEX 2-73 and ANAVEX PLUS. Phase 2a
Sigma2 receptor (progesterone receptor membrane component 1) inhibitor
- CogRx: CT0109, CT0093, CT01344, and CT01346. Block soluble Abeta oligomer-induced toxicity on synapses. Preclinical
RAGE (Receptors for Advanced Glycated Endproducts) inhibition
- vTv Therapeutics: Azeliragon (TTP488). Phase 3 for mild Alzheimer's
Fyn kinase inhibition
- AstraZeneca: AZD0530 (saracatinib). Phase 2. (Also possible MS)
PPAR-γ (Peroxisome Proliferator–Activated Receptor γ) agonist
- Takeda/Zinfandel: AD4833 (pioglitazone, 2,4-Thiazolidinedione, Actos, Glustin, Piozone). Phase 3 (began 2013), Alzheimer’s Mild Cognitive Impairment. Approved for Type 2 diabetes mellitus.
Metabolic Stimulation (ketones substituting for glucose to promote metabolism of fats)
- Accera: AC-1204. Phase 3 clinical trials, mild to moderate AD
General Amyloid Interaction Motif (GAIM)
- NeuroPhage Pharmaceuticals: NPT088. Preclinical
Anti-immuno senescence (Active immunotherapy)
- AC Immune SA, Janssen: ACI-35. Phase 1
- AC Immune SA: ACI-24 (Pal1-15 acetate salt). Alzheimer's disease Phase 1/2, Down's Syndrome. Phase 1
- Novartis: CAD106. Phase 2/3
Anti-Tau (NFT: neurofibrillary tangles)
Small Molecule (prevent or dissolve tau aggregation)
- TauRx: LMTX (leuco-methylthioninium). Two Phase 2 trials; data second half 2016 (mild, mild-to-moderate). Enrolling Phase 3, Alzheimer's disease, Frontotemporal Dementia
- Ogliomerix: Tau Oligomer Inhibitor; Tau Protease Inhibitor; Biomarkers for both programs. Alzheimer’s, Preclinical
Immunotherapy (Active)
- AC Immune SA, Janssen: ACI-35. Phase 1
- Axon Neuroscience SE: AADvac-1
SYMPTOMS/NEURAL HEALTH
Anti-cholinergic
- Eisai/Pfizer: Aricept (donezepil). FDA approved 1996
- Also approved: Razadyne (galantamine), Exelon (rivastigmine), and Cognex (tacrine)1
N-methyl-D-aspartate (NMDA) blockade
- Actavis: Namenda (memantine). FDA approved 2003
Type 4 phosphodiesterases (PDE4) inhibition
- Tetra Discovery Partners: BPN14770. Phase 2
5-hydroxytraptamine-6 (5-HT6) Antagonists
- Axovant Sciences: RVT-101. Phase 3 (with donepezil)
- Lundbeck & Otsuka America Pharmaceutical: AE58054 Phase 3; Others: four in Phase 2; three in Phase 1
- Pfizer: PF-05212377. Phase 2 discontinued, October 2015
Neuroprotection/Neurogenesis
- Amarantus: MANF (mesencephalic- astrocyte-derived neurotrophic factor), Preclinical
- M3 Biotechnology, MM-201 – Modified Neurotrophic Factor, Preclinical
ALZHEIMER’S ADVANCES — DEVELOPMENT DURING DEBATE
“The hallmark pathologies of Alzheimer’s are the progressive accumulation of the protein fragment beta-amyloid (plaques) outside neurons in the brain and twisted strands of the protein tau (tangles) inside neurons. These changes are eventually accompanied by the damage and death of neurons.” Alzheimer’s Association Facts & Figures 2015.
Most likely, there is no one in this field without a stake in the development of some specific approach or agent. Nevertheless, the KOLs who participated in this virtual roundtable gave fair and widely focused views of current scientific thought in the ND area. Not that the field harbors uniform consensus. For every hypothesis about the progression of Alzheimer’s, a contrary assertion seems plausible. Is Alzheimer’s all about the accumulation of beta amyloid plaque? If so, why do so many people who never get the disease walk around with massive amounts of plaque in their brains? On the other hand, why did some patients with advanced disease seem to benefit from plaquetargeting mAbs (monoclonal antibodies) that produced poor overall results in Phase 3 trials?
It’s important to note, however, that the Phase 3 trials have mostly happened under the wing of a Big Pharma company. It has been 20 years since the approval of Aricept (donezepil), the last major advancement in Alzheimer’s therapy, however modest in effect. Lilly, Biogen, and Roche have all had their setbacks, but seem committed to the long haul, though Pfizer and Janssen have discontinued their late-stage programs. Still, it is now clear that ND drug development is no longer the lonely pilgrimage of small companies.
Beyond anti-amyloid, the next most powerful camp in scientific thinking is anti-tau, specifically, phosphorylated tau tangles. Tau proteins are normally straight and parallel fibers that stabilize microtubules inside neurons. Like the rails ripped up and left hopelessly tangled by Union troops as they marched through Georgia, tau fibers in Alzheimer’s patients typically become “hyper-phosphorylated,” or overwhelmed in binding with phosphoryl groups, detach from the microtubules, and misfold and intertwine, killing the neurons.
Anti-tauists point to the closer association of tau tangles with cell death and cognitive decline. But the pathway that leads to toxic Abeta plaque and tau tangles is the same — an evolutionary sequence that may encompass all the key steps in development of the human brain and its higher functions of thought and memory, yet somehow working in reverse to degenerate the same structures. Almost all of the key points along the pathway have become targets of new therapeutic strategies and mechanisms for Alzheimer’s — much like the continuum of checkpoints in immuno-oncology. A fair number of those targets, strategies, and mechanisms may apply to other NDs as well.
But disease modification is only one of the goals for new Alzheimer’s drugs. Much of the R&D effort in this space goes toward developing better agents for relieving symptoms or compensating for lost neurons and synapses by enhancing neurotransmission, delivering neuroprotection, or even promoting neuroregeneration. At the same time, as the Alzheimer’s experts in this article emphasize, education in both the academic and public relations senses may still be the most powerful and essential tool available for preventing, forestalling, and treating the disease.
All of the new treatment approaches have one thing in common: the importance of early diagnosis and diagnostic tools. Another common denominator is drug delivery past the bloodbrain barrier, and a quick search of Life Science Leader and its sister Web portals will yield much on those topics. Imaging and blood testing for disease biomarkers have advanced, but so far they are mainly focused on amyloid plaque, and behind that, tau, and there is little that would guide use of drugs with other mechanisms. Diagnostics especially deserve their own chapter in this story. But the truth is, methods for detecting the earliest stages of Alzheimer’s are still a long way from feasible and affordable availability and use.
