Renewed Focus On Prevention Is Necessary To Improve Population Well Being
By Suresh Kumar
 Will 2020 be the year when public and political discourse anchors healthcare policy in fact-based epidemiology? Will it be the year when the ways in which healthcare policies are shaped address the root causes of illness? Could it be the year when policy gets based on a ruthless examination of past learnings (what works/what does not), the present (whether current programs drive or detract from national health), and the future (how science, technology, and behavioral science can be leveraged to affordably combat onset and cure of disease)? Lower prevalence of disease defines well-being. Moving from sick care to healthcare means focusing beyond the cure on prevention and abatement of disease. This has been the basis for vaccination programs from infancy through later years. A greater focus to influence and embed a healthier lifestyle is required now — what we eat and drink and how we move and rest impact well-being more than anything else. After all, how long can the U.S. afford the current trajectory of illness and healthcare outcomes?
Will 2020 be the year when public and political discourse anchors healthcare policy in fact-based epidemiology? Will it be the year when the ways in which healthcare policies are shaped address the root causes of illness? Could it be the year when policy gets based on a ruthless examination of past learnings (what works/what does not), the present (whether current programs drive or detract from national health), and the future (how science, technology, and behavioral science can be leveraged to affordably combat onset and cure of disease)? Lower prevalence of disease defines well-being. Moving from sick care to healthcare means focusing beyond the cure on prevention and abatement of disease. This has been the basis for vaccination programs from infancy through later years. A greater focus to influence and embed a healthier lifestyle is required now — what we eat and drink and how we move and rest impact well-being more than anything else. After all, how long can the U.S. afford the current trajectory of illness and healthcare outcomes?
FACE REALITY: ILLNESS IS RAMPANT IN THE U.S., AND OUTCOMES SHOW LITTLE PROGRESS!
Six out of 10 adults in U.S. have a chronic disease and four in 10 have two or more. These patients account for 90 percent of all healthcare spending. Approximately, 122 million have cardiovascular disease that results in 840,000 annual deaths. Nearly 30 million Americans have diabetes, and another 84 million are prediabetic, a ticking time bomb — but one that can be alleviated with the right efforts. In 2016, the direct and indirect cost of chronic disease that was influenced by obesity was $1.72 trillion, i.e., 9.3 percent of the GDP. The latest National Health and Nutrition Examination Survey (NHANES) states that 40 percent of adults and 19 percent of children between ages 2 and 19 are obese — the highest ever recorded in their survey.
Nutrition, physical activity, mental health, and substance abuse disorders are key causal factors of our chronic diseases and must be targeted as part of any public health policy that aims to arrest the trajectory of disease and improve population well-being.
RECENT POLICY INTERVENTIONS IMPERIL PROGRESS
Ironically, when interests of people collide with those of corporations, the latter invariably prevails as evidenced by recent examples of U.S.-led policy interventions.
- In the New NAFTA, the U.S. made concerted efforts to get Mexico and Canada to roll back public health-interest-led food labelling to combat obesity and promote healthy consumption via instantly recognizable front-of-package symbols. Although public outcry and Congressional grilling thwarted explicit antilabelling provisions (desired by the administration and the food lobby) from making it into the final agreement, those objections could not arrest other plans intended to dilute regulations, including provisions that limit information on food ingredients, additives, and nutrition and even omit ultraprocessed food from bioengineered drug labelling. Mexico and Canada led the way in putting people and public health first — the U.S. opted to be the “megaphone of the food lobby.” Consumers need noticeable and understandable information on product labels, such as product safety and sugar, salt, and fat content information, to guide toward purchasing, healthier choices, and, ultimately, modifying behavior. This kind of information is impossible to miss on the front labels of products sold in Canada and Mexico. Information for the same brands sold in the U.S. is buried in small fonts and fine print on the back label.
Treaty harmonization must secure and improve public health, not impose labelling hurdles where “technical-barriers-to-trade” rules can be imposed to uphold U.S. food-lobby interests over shaping healthier choices.
- A pro-breastfeeding resolution at the United Nations was expected to pass unanimously at the UN Health Assembly until U.S. administration attempted to derail it — and go beyond to actually threaten indebted nations like Ecuador that supported the initiative — with withdrawal of military and other support. Worse, the administration originally sought to remove “protect, promote and support breastfeeding” and “restrict promoting food that can be harmful to young children” from the resolution. Almost 50 years of research has established that breast milk provides essential nutrients, hormones, and antibodies that protect newborns against infectious disease. A 2016 study in The Lancet found that universal breastfeeding would prevent 800,000 child deaths annually worldwide and yield $300 billion in savings from reduced healthcare costs and improved economic outcomes for those reared on breast milk. Scientists felt that undertaking U.S. double-blind study protocols for “evidence-based” research was ethically and morally unacceptable, as it entailed providing one group with breast milk and another with breast milk substitutes. Global outcry and a Russia-sponsored compromise resulted in a diluted resolution that requires the WHO to support governments trying to stop “inappropriate promotion of foods for infants and young children”. The moral high ground was ceded on a global stage in a way that no subsequent presidential tweet could sway.
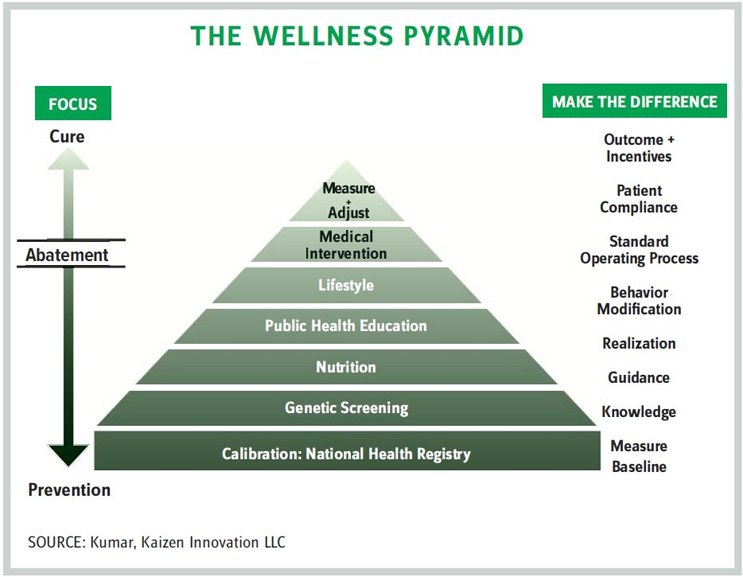
THE JOURNEY FROM SICKNESS TO WELLNESS
Healthcare is multifaceted, and we all know that governments influence how people and businesses behave. Individual behaviors such as eating, drinking, exercise, and sleep habits all impact public health. Regulations shape corporate behavior. Similarly, the public’s health, safety, and well-being are impacted by the transparency associated with a product’s contents, price, and risks associated with its use. Policy stewardship shines a spotlight on people and patients, works for the common good first, and — notwithstanding the administration’s recent performance — addresses commercial interests next.
The goal of progressive public health policies is to transition populations from sickness to wellness by aiming to:
- prevent or delay the onset of disease
- reduce the severity of disease and disability
- shorten periods of treatment and cure.
Regressing the trajectory of disease will encompass:
- genetic screening, genomics, and gene editing — all of which are designed to establish a baseline and calibrate health risks in the population
- lifestyle modification and medical intervention — all of which are encapsulated in a technology-driven feedback loop that calibrates and measures outcomes (see figure at left)
- nutrition — what to eat and drink, what to reduce or avoid, and how this information is disseminated
- public health education and guidance on:
a. healthy eating and drinking
b. physical fitness, exercise, and getting America to move at home, at school, and at work.
c. mental well-being, determining and reducing stress levels of our society
d. calibrating how rested or agitated we are. While this is complex, technology enables measuring one marker — sleep
e. determining the trajectory and causes of substance abuse and stress torque in a society
f. establishing if screen and typing time pose addiction risk (the ubiquity of mobile phones and technology warrants better understanding of risks such as blue light and vison, time on keyboards, and carpal tunnel syndrome).
THE ROAD MAP TO REALITY
A good journey begins with questions to identify a destination and build an itinerary. You be the judge: Are our public health policy initiatives appropriate, effective, and affordable? Are they in sync with our demographic and epidemiological trends? Can they bend the trajectory of disease and the healthcare cost curve?
SURESH KUMAR serves on the board of Jubilant Pharmaceuticals and Medocity. Formerly, he was U.S. assistant secretary of commerce and executive VP at Sanofi.
