A Realistic Look At What RFK Jr. Could Mean For FDA
By Jennifer D. Newberger and Jeffrey N. Gibbs, Hyman, Phelps, & McNamara
"A version of this article was published first on Hyman, Phelps & McNamara’s FDA Law Blog. It is republished here with permission."
In November, President-Elect Trump announced his pick of Robert Kennedy, Jr., for Secretary of Health and Human Services (HHS). Although not altogether surprising, the formality of an official announcement still came as a shock to many of us who work in areas regulated by HHS, as well as to many others in the public health arena.
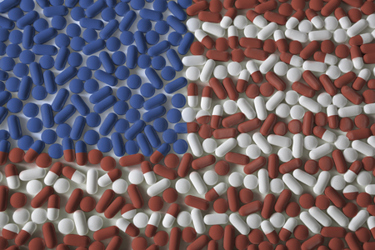
Kennedy’s tag line is that he and Trump will “Make America Healthy Again.” This seems like a reasonable goal, as most people can probably agree that America is not healthy. Rates of chronic disease are high, as is obesity. Incentives to motivate better nutritional choices and increase physical fitness would be welcome.
The question, however, is how Kennedy plans to accomplish this generally accepted goal. Some insights come from an op-ed Kennedy wrote in the Wall Street Journal on September 5, 2024, setting forth some of his plans for a healthier America. The first point he made pertained to reforming the Prescription Drug User Fee Act (PDUFA). He states, correctly, that PDUFA user fees make up about 75% of the budget for the FDA’s CDER. Though he did not mention it, there is also a Medical Device User Fee Act (MDUFA), which accounted for approximately 44% of the budget for the FDA’s Center for Devices and Radiological Health (CDRH) in FY2023. Kennedy stated that payment of these user fees by industry “creates a barrier to entry to smaller firms and puts bureaucrats’ purse strings in the hands of the pharmaceutical industry.” Kennedy does not say what the alternative to user fees would be given current budget realities.
It seems Kennedy is unaware of the waivers or fee reductions available to small businesses, both for drug and device submissions, precisely to avoid creating a barrier to entry. The second part of Kennedy’s statement expresses concern that because companies are essentially paying the salaries of the review teams, that the teams somehow feel obligated to approve the products.
On this second point, Kennedy elsewhere contradicts his own assertion that user fees lead reviewers to feel beholden to sponsors. Kennedy has stated that FDA’s recent denial of the psychedelic drug MDMA to treat PTSD constitutes “aggressive suppression of psychedelics” and has listed it as among the regulatory decisions he wants to reverse. If FDA reviewers felt obliged to accommodate the payers of the user fees, it is not clear why this — and many other drugs and devices — would have been rejected. (Based on our own experiences, we can confidently say that FDA reviewers are not rubber-stamping applications because sponsors pay user fees.) One possible explanation for this apparent contradiction is that in the case of approved drugs that he does not believe should have been approved, they must only have been approved because FDA is in industry’s pocket. On the flip side, in the case of drugs that he believes should have been approved but were not, FDA is waging a “war on public health.”
Belief, anecdote, and opinion seem to be the driving factor behind much of Kennedy’s rhetoric. The New York Post, not known for its Democratic leanings, stated in an article published on November 14 that installing Kennedy as the head of HHS breaks the most important rule of medicine: first, do no harm. Referencing an interview with Kennedy from 2023, the Post says that his views on health “were a head-scratching spaghetti of what we can only call warped conspiracy theories, and not just on vaccines.” They note his position that pesticides, cellphones, and ultrasound “could be driving an upswing in Tourette syndrome and peanut allergies,” and that “all America’s chronic health problems began in one year in the 1980s when a dozen bad things happened.”
The positions he espouses seem to have no grounding in scientific evidence or data. His well-known anti-vaccine stance is in stark contrast to decades of scientific research demonstrating the positive impacts of vaccination globally. He has equated vaccination to the Holocaust and argued that COVID-19 was “ethnically targeted” to spare Ashkenazi Jews and the Chinese. He has stated that ivermectin and hydroxychloroquine are effective COVID treatments, notwithstanding evidence to the contrary.
Given the above, the obvious question seems to be: what will be the role of science in an FDA under Kennedy’s leadership? Science is, at its core, a place to ask questions, to challenge norms, and to make new discoveries, and then to subject those discoveries to replication in a controlled manner. Galen’s belief in the four humors was sincere and deeply held, and also deeply wrong, as evidence-based science eventually showed. In the meantime, this belief was followed for centuries by doctors, to the detriment of countless patients.
FDA Grounds Its Very Existence In The Principles Of Science
According to an FDA statement on scientific integrity, “Science — both its quality and integrity — is the touchstone of everything we do at FDA. In conducting our mission to protect, promote, and advance the public health, FDA needs the best scientific and technological information available to make decisions on the products we regulate. Critical to our ability to reach sound decisions and to retain the public’s trust are high-quality data and a scientific review process that is thorough and unbiased.”
Kennedy’s pronouncements raise serious concerns as to whether scientific evidence and clinical data will continue to serve as the principles by which FDA makes critical decisions each and every day, or whether his beliefs — or the beliefs of new FDA officials he gets to select — will drive FDA decisions.
The potential consequences could be severe. CDRH’s long-standing definition of “valid scientific evidence” does not include opinions or beliefs. Indeed, it explicitly excludes “random experiences” and “isolated case reports,” which seem to be the kinds of “evidence” that Kennedy is willing to rely upon when making his pronouncements.
Public confidence in the device review process is already fragile. It relies on the belief that FDA carefully considers the safety and effectiveness of devices. The public’s faith in the process is already severely challenged by critics who argue that the process is lax — and whose views are widely reported. Substantially weakening the data standards would likely cause significant erosion in public trust. It would also undercut CDRH’s position as being a gold standard for the review process, which benefits U.S. companies seeking to market their devices abroad. Moreover, Congress has established data standards for device review. Kennedy could not unilaterally change those congressional criteria; personal beliefs do not qualify as “adequate assurance of safety and effectiveness.”
It is worth noting that the Secretary of HHS is responsible for many tasks and agencies apart from FDA, and generally has very little influence over the day-to-day review decisions. Thus, while FDA is foremost in our mind, it may not be in his. Even so, his perspectives on the roles of science and belief could be transmitted to FDA.
The individual tasked with overseeing the agencies responsible for protecting the public’s health should endorse the role of science, not disparage it. Whether a Kennedy regime would base its decisions on science rather than belief remains to be seen, but his words and public pronouncements to date are not encouraging, although his views could possibly shift — to some degree. Wise government officials will modulate their views as they learn new facts.
 About The Authors:
About The Authors:
Jennifer Newberger is a director at Hyman, Phelps & McNamara where she provides counsel to medical device manufacturers on matters including regulatory strategy, submissions, and enforcement matters related to the FDA and other agencies, including the Justice Department. She worked for the firm from 2011 to 2017 and left temporarily for posts at Apple, Abbott Laboratories, and Cognito Therapeutics. She returned to HPM in 2024.
 Jeffrey Gibbs is a director at Hyman, Phelps & McNamara where he supports companies on FDA issues. He began his career with the firm in 1990 and has written and lectured on a number of agency-related topics including medical devices, in vitro diagnostics, and enforcement. Previously, he was associate general counsel for enforcement at the FDA. He was appointed special assistant U.S. Attorney for the District of Columbia and earlier clerked for a U.S. District Court judge in New Jersey.
Jeffrey Gibbs is a director at Hyman, Phelps & McNamara where he supports companies on FDA issues. He began his career with the firm in 1990 and has written and lectured on a number of agency-related topics including medical devices, in vitro diagnostics, and enforcement. Previously, he was associate general counsel for enforcement at the FDA. He was appointed special assistant U.S. Attorney for the District of Columbia and earlier clerked for a U.S. District Court judge in New Jersey.
