Collaborations Trump Competition During Pandemics
By Suresh Kumar
Figures as of April 27th, 2020
 The U.S. was not unaware of COVID-19 — it was unprepared. How could a country this resourceful and rich go so wrong, so quickly? Unreliable and inept federal leadership, belligerent and untrustworthy communications, and flat-footed institutions all compromise coalitions. This President’s “I-win-you-lose, me-good-you bad” demeanor alienates allies. His disregard for own his government’s safety protocols defies science and denigrates experts. The President’s irresponsible suggestions to inject or ingest disinfectants as protection against COVID-19 prompted record calls from concerned citizens to the nation’s Poison Control Centers. While viruses endanger people, presidential tweets that incite people to disregard public health protocols poisons the populace.
The U.S. was not unaware of COVID-19 — it was unprepared. How could a country this resourceful and rich go so wrong, so quickly? Unreliable and inept federal leadership, belligerent and untrustworthy communications, and flat-footed institutions all compromise coalitions. This President’s “I-win-you-lose, me-good-you bad” demeanor alienates allies. His disregard for own his government’s safety protocols defies science and denigrates experts. The President’s irresponsible suggestions to inject or ingest disinfectants as protection against COVID-19 prompted record calls from concerned citizens to the nation’s Poison Control Centers. While viruses endanger people, presidential tweets that incite people to disregard public health protocols poisons the populace.
This column is a retrospective and prospective on how institutions and infrastructure must evolve to manage essential supplies that protect Americans.
The Here and Now: Put Tests To Rest
The threat of COVID-19, known before Christmas, was downplayed by the President through January. By February sanitizers and hand wipes had flown off retail shelves, and by March stores were running out of toilet paper. Critical supplies fared worse: The U.S. remains woefully short of supplies such as testing kits, swabs, reagents, protective equipment, and ventilators.
The internet enables instant dissemination of information to speed development. Chinese scientists published the COVID-19 genome on Jan. 12. By Jan. 21 WHO posted the blueprint for a test that laboratories around the world could duplicate. As regulators worldwide rapidly approved tests and testing protocols, U.S. healthcare agencies vexingly stuck to a not invented here (sic, NIH) syndrome. The CDC pursued its own test, and the FDA delayed collaborating with the private sector to commercialize tests. Symmetry in failure across multiple public health agencies in not accidental; it points to a deliberate White House focus away from healthcare investments. The administration wouldn’t announce expanded testing until March. By April 16, time lost to test, isolate, and treat COVID-19 patients had claimed 56,180 American lives versus 6,021 in Germany. Only 5.6 million Americans —13,000 per million — were tested versus 25,000/MN levels in Germany and Italy, and 20,000 in Spain. From a Harvard study projection requiring between 500,000 to 700,000 tests/day, to Paul Romer’s goal of testing 7 percent of U.S. population daily, most studies require a fivefold increase in testing to safely open the economy. Perfecting and testing at scale for infection and for antibodies is necessary to identify a “clean” population that can safely go back to work. Besides, the antibody test is yet to be perfected and false negatives risk resurgence. Recurring tests and stockpiled testing supplies will be required until preventive or curative therapies become available to ensure that workers remain COVID-19 free.
With 4 percent of the world’s population, the U.S. accounts for over 32 percent of infections and 26 percent of COVID-19 related deaths. The President’s gloating over his administration’s “great performance” through the pandemic is delusional. The media has a responsibility to call this out and stop covering daily political rallies replete with lies that masquerade as White House briefings. The inability to build cohesive policies, operational strategies, and global/state/local-level collaborations compromised our ability to secure supplies of life-supporting equipment. It jeopardized public safety, caused economic anguish, and claimed American lives.
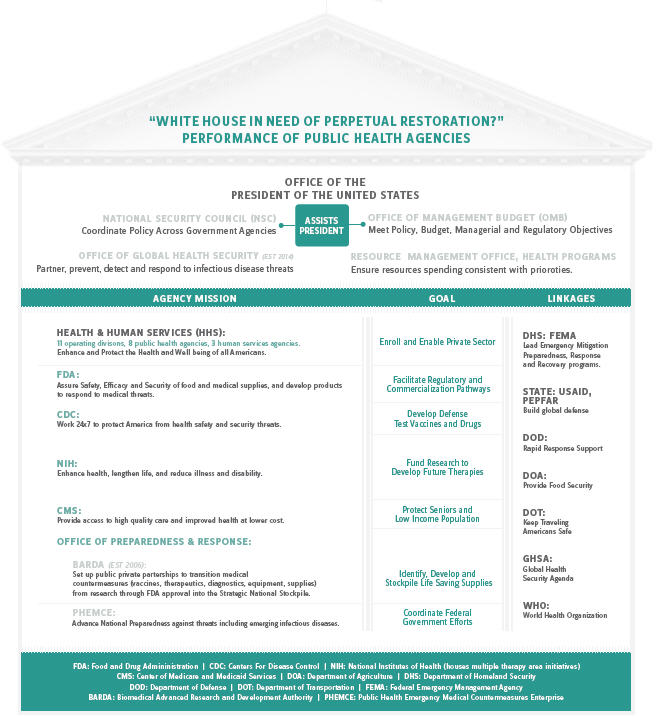
The Role Of Government & Public Health Institutions
No one could have predicted the scale of COVID-19’s rapid spread, and despite more frequent epidemic occurrences (see my ) public health institutions have remained historically under-resourced. Previous presidents, however, foresaw the threat of infectious disease and strengthened public safety infrastructure: Bush established PEPFAR (2003) and BARDA (2006) to strengthen the Strategic National Stockpile (SNS). Obama established the Office of Global Health Security (2014) within the National Security Council to enable a White House-level coordinated rapid response to keep America safe. The Trump administration dismantled or impaired these offices and initiatives, even proposing Congress take back $252MN allocated to Zika rather than repurposing this for pressing public health needs. Responsibility for public health is dispersed across a labyrinth of agencies with well-defined purposes — U.S. Departments of Health, Homeland Security, Defense, Veterans Affairs, State, Transportation, Agriculture, and Interior. Lack of a single point of ownership compromises ability to marshal resources and respond with alacrity.
The current approach to national security focusing on defense to the exclusion of almost all else is myopic. It conjures images of cavalier cowboys from the wild west running the West Wing. Fixating on building physical walls and weaponry and on repealing healthcare benefits cannot contain pandemics or keep our sailors and soldiers immune to viral or digital attacks. Doing so has compromised frontline warriors — medical workers who fight COVID-19 without personal protection equipment.
President Eisenhower famously called defense spending the “Military Industrial Complex.” The 2020 Defense Budget of $718BN has redundancies that may enable fighting multiple wars but cannot keep Americans safe while investments in public health remain cockily negligible: $2.6BN for preparedness and response, $12.8BN for discretionary programs at the CDC, and $5.9BN at the FDA. What gets budgeted gets done. A feast-or-famine approach to funding national security risks American lives.
How Taxes Are Deployed To Secure Supply Chains That Keep Americans Safe
Public health is part of national security, and urban planning is integral to public health. Futuristic? Prudent?
Supply chains are means tested for affordability and to determine budgetary adjustments necessary to deliver national security goals. Supply chains are also tested for vulnerabilities — e.g., EOQ (economic order quantity), MOQ (minimum order quantity), safety and surge levels, and sourcing concentration and delivery lead time risks that warrant developing supplemental sources of supply. Technical and economic evaluations need to be concurrent across the supply chain; this is rare within government contracting regulations that need updating. Military-like exercises establish supply chain risks and promote vigilance. This administration ignored outcomes and risks that surfaced in its own simulations. (Listen to NPR’s All Things Considered from March 20,2020 , “What Last year’s Government Simulation Predicted About Today’s Pandemic.”)
High dependence on global healthcare supply chains were highlighted earlier (See my January 2019 column). Outsourcing to lower cost of goods can be considered only if the risks are addressed (e.g., demand forecast lead times and order cycles, establishing supplemental sources for emergency supplies). Additional FDA resources are necessary to ensure integrity and continuity of critical offshore supplies such as food, medicines, and medical equipment.
Everything begins with realistic budgets to source and hold established levels of critical supplies in the SNS. In the battle against COVID-19, these include:
- Personal protection equipment (PPE) — Production of masks, gowns, caps, shoe covers, protective glasses, etc. migrated from the U.S. to China and emerging markets because of lower cost of goods. Supplemental supply sources for emergency surges need to be established.
- Ventilators — The U.S. needs 70,000 additional ventilators; the SNS has only 12,600. Local development has remained elusive. Criticizing countries that supply ventilators risks exacerbating the situation.
- Medical workers — We need to recalibrate need vs. availability by geography and address how demand surges will be met. Establishing a National Guard-like auxiliary healthcare workforce should be seriously considered.
- Hospital beds for meeting demand surges — Design, specifications, and prototypes of temporary field hospitals and ambulatory units to supplement permanent structures must be established, budgeted within the SNS, and procurement contracts issued.
How We Got Here, And How We Must Get Out
In this administration, economy trumps healthcare, corporate interests trump people, profits trump public safety, innuendoes trump reality, and belligerence trumps engendering trust. Healthy Americans are prerequisites for a strong America, and adequate testing is the rate-limiting factor to opening the economy. Fiscal and monetary bailouts, while essential to stabilize America now, must be followed by clear guidelines on how they will be paid for and how taxes will be generated and deployed in the future to keep our economy safe and resilient. America Inc. only works when we regain our fiscal balance, global standing, and moral high ground.
SURESH KUMAR serves on the board of Jubilant Pharmaceuticals and Medocity. Formerly, he was U.S. assistant secretary of Commerce and executive VP at Sanofi.