Demographically Appropriate Policies Deliver Sustainable Care And Healthy Populations
By Suresh Kumar
 Demographics, more than anything else, determine the appropriateness of healthcare policies. In 2019, the U.S. recorded its lowest population growth in a century. The challenge of an aging population with fewer women of child-bearing age and fewer registered births was compounded by immigration declining to half the level it was in 2016. One year does not make a trend but raises red flags in policy approaches. Most economists agree that a healthy and growing population is necessary to sustain vibrant economies. Prosperous nations need working-age populations to produce products and services, contribute to essential programs, sustain consumer spending, and spur commerce. These are all necessary to support a U.S. population that will top 400 million by 2050. Playing politics with policy risks impairing prosperity. Are current healthcare policies effective to keep future generations of Americans physically, biologically, economically, and emotionally secure?
Demographics, more than anything else, determine the appropriateness of healthcare policies. In 2019, the U.S. recorded its lowest population growth in a century. The challenge of an aging population with fewer women of child-bearing age and fewer registered births was compounded by immigration declining to half the level it was in 2016. One year does not make a trend but raises red flags in policy approaches. Most economists agree that a healthy and growing population is necessary to sustain vibrant economies. Prosperous nations need working-age populations to produce products and services, contribute to essential programs, sustain consumer spending, and spur commerce. These are all necessary to support a U.S. population that will top 400 million by 2050. Playing politics with policy risks impairing prosperity. Are current healthcare policies effective to keep future generations of Americans physically, biologically, economically, and emotionally secure?
DEMOGRAPHIC FUNDAMENTALS - THE BUILDING BLOCKS FOR FUTURE SECURITY AND PROSPERITY
Population is the building block of demographics. In a healthy population, annual births plus immigration exceed deaths. U.S. population growth is in secular decline: Last year the U.S. added just over 1.5 million people or 0.5 percent versus over 1 percent annual growth in the 1990s, under 1 percent in the decade ending 2010, 0.7 percent between 2010 and 2015, and 0.6 percent in the last five years. Reversing this trend will require higher birth rates in existing and new immigration populations and increased immigration. Lately, too much emphasis has been placed on population divisions by race, color, religion, and ethnicity without an appreciation for the economic impact of population changes on national health programs or on population levels necessary to sustain economic growth and healthy well-being.
A crucial measure of sustainable economic and social progress is the Dependency Ratio, which measures the number of dependents, typically those in school until the age of 15, and retirees over age 65, as a proportion of the working population. This has been adjusted to:
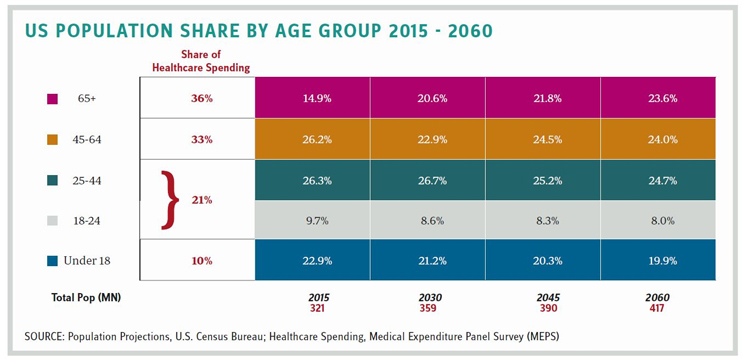
Adjustment of dependency from 15 to 18 years is warranted based on when most children transition from school and university to the workforce. This adjusted dependency ratio will grow from 61 percent in 2015 to 76 percent in 2060. Today’s 65+ population helped pay for the education of the current working-age group, and past generations of retirees continue to pay Medicare Part B and D premiums, and some of them continue to work. All of this alleviates the economic burden on society. Nevertheless, older people account for a disproportionate cost of care, and an aging population and falling birth rate result in growing dependency (See Table). Smart healthcare policies are acutely needed now to alter the trajectory of disease and embed therapies, treatments, and behavioral adjustments to improve health. Innovative science-, technology-, and genomics-driven prevention therapies must complement public health and education programs to modify diet, nutrition, and physical and mental acuity levels.
INNOVATION HAPPENS AT THE FRINGE, BEFORE GOING MAINSTREAM
Resistance to reinventing the core of healthcare results in policy gridlock. An alternate approach is to demonstrate the ability to alter practices in dependent care for child, youth, and elderly populations (38 percent today that is projected to grow to 43 percent of U.S. population by 2060). This month’s column focuses on rethinking needs of the “numerator populations” in the dependency ratio to accelerate innovation in prevention and maintenance of disease. This will allow quicker demonstration of superior outcomes to inspire confidence for mainstream changes.
ADOLESCENT AND YOUTH WELL-BEING:
Scientific and technological advances in genomics open pathways for innovative therapies, treatments, and procedures that can retard incidence and eventually eliminate some congenital and rare diseases. The current approach to treating rare disease (i.e., conditions that affect less than 200,000 patients) with orphan drugs that cost more than $106,000 per year (estimate from 2017 at drug launch) exacerbates the healthcare challenge. Mandating premarital and newborn screening can preempt disease and enable early identification and treatment of at-risk populations. This will help decrease patients’ suffering, parental anguish, and the cost of healthcare. Policy frameworks that mandate testing will be required along with establishing protocols for testing, treatment, secure data collection, analytics, protection, and storage. Principles governing patient-data ownership and consent for use of data in unidentifiable aggregation (for use in research and development) must also be established. Together these policies and protocols will facilitate broader patient access to scientific and technological innovations and help create a healthy youth population.
Public health initiatives to educate children and parents on diet and nutrition, incorporating physical exercise in school curriculum, and mandating foods and beverages that can be dispensed at schools can arrest the scourge of obesity and reduce metabolic disease and disorders. Together these interventions can influence healthy adolescent and adult behaviors and reduce future cost burden.
KEEPING SENIOR CITIZENS HEALTHY AND RETHINKING ELDER HEALTH
People 65 years+ are already 15 percent of the U.S. population. Increasingly active, they live longer and account for 36 percent of all healthcare spending. Keeping them healthy and engaged must be a priority and will require a major rethink on how care is delivered. The elderly are not a monolithic group. They exhibit a variety of life-stage needs: socially active and living with a spouse, when assistance is required to stay agile, and later years when assistance is needed with regular chores and activities of daily living. Elder care requires health maintenance via timely care delivery. It requires high- and low-tech innovation: technology that enables remote tracking of daily activity, vital signs and a person’s compliance with diet, exercise, and medication regimens. Personalized care in later life stages combines technology with community-based care and access to concierge-like services and periodic doctor visits. Insurance coverage needs rethinking from what is covered to how care is delivered. Would coverage for vision, hearing, dental, and physical therapy — among others — improve daily functioning and quality of life? Could these preempt more expensive treatments? Could community-based care be a better way to keep the elderly happier and in proximity to friends and family? Could these be cheaper alternatives to expensive care at nursing homes?
THE BOTTOM LINE:
Critically reassessing changing demographics and listening to people and patients can help create innovative products, services, and solutions. Age-appropriate patient care can deliver greater patient satisfaction and better outcomes at lower cost. Isn’t this what we should aspire to? Without such aspiration, a declining proportion of working-age Americans will be unable to support the elderly or young adolescents who are tomorrow’s workforce.
SURESH KUMAR serves on the board of Jubilant Pharmaceuticals and Medocity. Formerly, he was U.S. Assistant Secretary of Commerce and Executive VP at Sanofi.
