Patient Satisfaction With Health Systems Is About Value, Not Just Cost
By Suresh Kumar
 International travels allow me to observe, contrast, and compare healthcare systems and services. This month’s travel across larger, more developed (E-5) European countries was more interactive and robust than usual. People living in universal healthcare regimes were intrigued by the “fuss on Medicare for all” and wanted to know “where is the U.S. headed — universal healthcare, a tribal fend-for-yourself model, or something only you guys can understand?”
International travels allow me to observe, contrast, and compare healthcare systems and services. This month’s travel across larger, more developed (E-5) European countries was more interactive and robust than usual. People living in universal healthcare regimes were intrigued by the “fuss on Medicare for all” and wanted to know “where is the U.S. headed — universal healthcare, a tribal fend-for-yourself model, or something only you guys can understand?”
Speaking with patients, consumers, global pharma executives, and local service providers is always informative. Observing independent doctors and vibrant auxiliary networks of audiologists, dentists, diagnostic laboratories, optometrists, and physiotherapists delivering more personalized healthcare services to increasingly older patient populations at public hospitals, private clinics, and other facilities in Europe was as revealing as the interviews with them were insightful. There was talk on policy and politics. There was discussion on costs and affordability. But all the conversations were grounded on delivering better patient care. The contrast between what is happening in Europe and the U.S. could not be more telling.
DISPELLING MYTHS
People and patients in the EU appear happier with their healthcare than those in the U.S. Can people and patients, not politicians and lobbyists, address healthcare needs and how it is delivered? When was the last such assessment done by CMS? The voice of patients must be more pronounced in national dialogue and framing policy. Should referendum-like questions on what people want for their healthcare be included on the ballot? A recent Pew Study reports 60 percent of Americans prefer universal healthcare compared to 51 percent in 2016: the likely effect of trying to repeal ACA without an alternative.
The goal of universal healthcare is increasing access where basic healthcare is egalitarian without regard to demographics, income, or status. Countries pursuing this goal require mandatory health insurance. There are no pure single payer systems. Most costs are funded by government, and some are paid for by employers or citizens via supplemental insurance. The issue at stake is who and what services are covered and how much cost is underwritten by government. In Europe, there is greater clarity in what is covered, what is not, and how much a doctor visit, a drug, or procedure costs. There is acknowledgement that patients must be consulted in designing healthcare systems, and that they must take responsibility for, and contribute toward, their healthcare. People want governments that underwrite the cost of healthcare to be empowered to negotiate prices — something that the U.S. does not do. EU citizens who spend less than the U.S. on healthcare are happier with their systems, benefits, and outcomes than their U.S. counterparts. Responsible stewardship of public resources entails strong oversight of private sector practices.
ACCEPTING FACTS
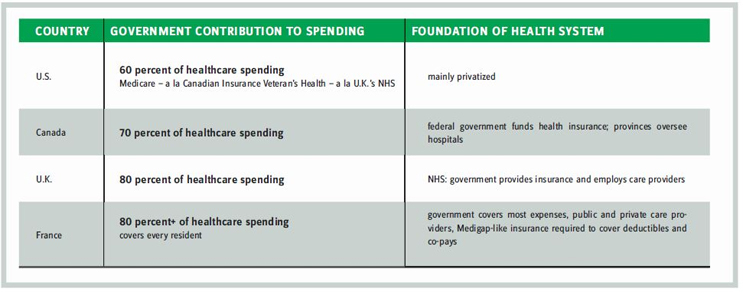
The U.S. spends $3.3 trillion (i.e., $10,348 per person) annually to provide care for 327 million people. The EU spends €1.1 trillion or 7 percent of GDP on 513 million people. A quick contrast of a few national systems is provided, with a guiding comment: Spending more on healthcare does not translate to better patient outcomes.
The EU healthcare system varies by country but is more fragmented than the U.S. Many services are delivered via private enterprise (e.g., clinics, physician practices, independent pharmacies, and care services relevant for the wellness of an aging population).
This is dispersed-capitalism where entrepreneur-run businesses provide superior and more relevant care for people, not vilified socialized medicine.
By contrast, lesser-fragmented U.S. healthcare continues to consolidate, concentrating more economic power in fewer institutions (e.g., provider facilities, insurers, and drug, device, or diagnostic companies) with the goal of improving negotiating clout to realize better economies of scale. Yet, the U.S. government, which underwrites 60 percent of healthcare spending, does not have authority to negotiate prices. This may serve politics and ideology, but it is poor policy and not patients’ or citizens’ best interest. Managed markets — where doctors prescribe, governments pay, and patients use — do not reflect consumer markets. Market power-based negotiating cannot be the prerogative of the private sector. Government agencies, i.e., Medicare, Medicaid, Defense, and Veteran Affairs, must jointly negotiate better prices for drugs, devices, and procedures and start to realize better outcomes. Only then will U.S. citizens not be held hostage to a system that results in 18 percent of GDP being spent on healthcare vs. 7 percent in OECD (Organization for Economic Co-operation and Development) countries.
Ironically, ideologues characterize European healthcare as socialized medicine, and skeptics blame drug cartel-like pricing practices for medicines and procedures on the lack of vibrant payer, provider, and pharma competition in the U.S. Facts, not rhetoric, and outcomes must guide policy.
IT IS NOT JUST COST, IT IS QUALITY, TOO
When discussion turns to healthcare, the French, Germans, and Spaniards have few complaints. Why? The following are some patient experiences — including my own — that I encountered during my recent visit.
I was not satisfied with the frame of my prescription glasses purchased in France two years ago, so the optician replaced the frame without any fuss. A friend with a small tear in his tendon was not pushed by scalpel-happy surgeons to a procedure; instead he was steered to several sessions with a kinesiologist and is back playing regular tennis. Endocrinologists spend 45-60 minutes counseling patients on diet, nutrition, exercise, and medication, and not on inputting readings into a computer in rushed 20-minute sessions as in the U.S. Two audiologists spent an hour testing and calibrating the hearing aid and running hearing tests. They determined that one of the Phonak aids covered under warranty for three years did not perform to standard and would be repaired or replaced. The testing is not as robust in the U. S., and warranties last just one year. In every instance, cost was not the issue; it was the attention to the patient’s interests that inevitably resulted in superior outcomes and value. No wonder most Europeans are happier with their healthcare than Americans are with theirs.
THE PHARMA PERSPECTIVE
Pharma professionals are riveted on what’s happening in healthcare in the U.S. and China, one a lucrative high-priced market and the industry’s profit driver, the other a volume growth engine. They are the industry’s lifeline, while EU is its nemesis. European governments have exercised greater formulary and fiscal control. Cost pressures will mount worldwide, and new products have struggled to reach more patients unless they are reasonably priced (e.g., high-priced cardiovascular products Entrestro, Repatha, and Praluent have all struggled to gain access). Two years after launch, Repatha and Praluent prices have been reduced by 60 percent. Industry is finally getting the message that price elasticity is finite even in the U.S. And I am observing early dissonance among executives on the industry’s aggressive lobbying tactics. It is time to think afresh, for newer business models with global appeal, where revenue and profits are not overtly reliant on the U. S. and China, but instead are globally generated.
Privatization is not the panacea for everything good, and government-led initiates are not always the culprit they are made out to be. A clear articulation of goals and transparency into coverage, cost, and value drive greater satisfaction.
SURESH KUMAR serves on the board of Jubilant Pharmaceuticals and Medocity. Formerly, he was U.S. Assistant Secretary of Commerce and executive VP at Sanofi
