Tackling The Challenges Of A Rare-Disease Clinical Trial
By Ed Miseta, Chief Editor, Clinical Leader
Regulatory agencies today are looking for Phase 3 trials to demonstrate a reduction in mortality as well as greater patient mobility. Unfortunately, Phase 3 trials also cost a lot of money to run, making them a challenge for small biotech firms. For a rare disease, the challenge is even greater, since patient recruitment is more difficult.
Jean-Louis Dasseux knows just how difficult it can be to run these trials. Dasseux is president and CEO of Cerenis Therapeutics, which is headquartered in France and focused on cures for cardiovascular disease (CVD). “Every year CVD results in the death of 17.3 million people, or one in every three deaths,” he explains. Current treatments, which attempt to lower low-density lipoprotein (LDL, also known as bad cholesterol), only reduce cardiovascular events by 25 to 35 percent. The drug in development by Cerenis attempts to mimic the role of natural high-density lipoprotein (HDL, also known as good cholesterol). Low levels of HDL caused by genetics have no current treatment and qualify as a rare disease.
“If we were hoping to reduce CVD events, we would have to perform an outcome trial that looked at the incidence of heart attack and stroke,” says Dasseux. “Those trials can last four or five years and would look for a reduction in the mortality rates in those patients. They are also very expensive and require 25,000 to 30,000 patients. That might be a good approach for companies with a lot of money, but not for a small biotech. As such, our strategy in the near term is to tackle a related rare disease. We are focused on fixing the absence of HDL caused by genetic defects.”
ONE PATIENT LEADS TO A PHASE 2 STUDY
Cerenis is currently running a Phase 3 clinical trial for patients suffering from two genetic defects that lead to very low levels of (or no) HDL. The company has come a long way from its start years ago when it embarked on an open-label Phase 2 study with just seven patients. The first patient, from a poor community in Sao Paulo, Brazil, had no HDL and was accumulating cholesterol everywhere in his body. Cerenis was contacted by the patient’s physician, who was aware of the company’s development efforts.
JEAN-LOUIS DASSEUX President & CEO, Cerenis Therapeutics
“We knew it would be difficult for a small organization to run a trial so far away,” says Dasseux. “We realized the preferred scenario would be for the patient to come to Europe. We worked with the Amsterdam Medical Center and were able to fly the patient from Brazil to Amsterdam for treatment. It was his first flight and he was scared, but he also had few options. With the accumulation of lipids he was experiencing, there were xanthoma, or lipids bumps, all over his body, and lipids in the vessel wall lead to heart attacks. He had three bypass surgeries and was getting worse.”
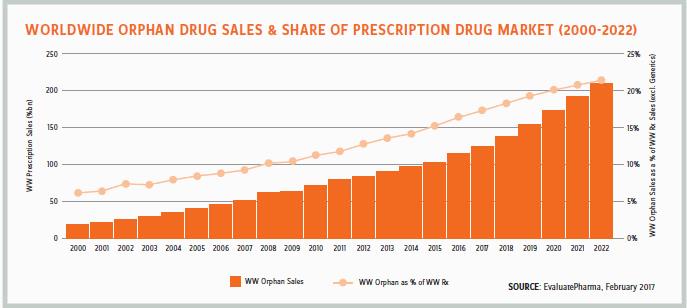
The treatment the patient received was effective, and Dasseux notes the drug was able to remove cholesterol from the vessel walls and eliminate it from the body. Based on those findings, seven patients were recruited to take part in the Phase 2 study. In that trial Cerenis demonstrated its ability to reduce the accumulation of lipids. Consequently, the European Medical Agency (EMA) granted two orphan drug designations to the company to fast track the study.
FINDING PATIENTS STILL A CHALLENGE
Patients with low HDL are not identified preemptively. If a patient happens to have a heart attack or CVD at a very young age, a blood test looking for low HDL is performed. This is how patients are identified for trials.
“Developing a drug for any rare disease is a challenge,” notes Dasseux. “Oftentimes you will be able to locate only one or two patients. You often have to go where the patients are, and that may mean running a trial in multiple countries, which creates additional challenges such as language barriers.”
To overcome the language problem, Cerenis works with local CROs for help filling out documents to get patients enrolled in trials. Those CROs also can assist with regulatory submissions. Still, Dasseux notes an even bigger challenge is making physicians aware that help is available for patients. This necessitates reaching out to physicians and clinics that might have potential candidates to let them know there is a drug that can treat the disease. To do so, Cerenis needs to build personal relationships with physicians. Part of that effort involves attending and speaking at conferences and getting on the radar of key opinion leaders to make them aware of study results.
The current Phase 3 study, named Tango, is ongoing and has 30 patients participating. Dasseux says there is a story behind each one getting involved with the trial. At one point he was contacted by a physician who had a potential subject who was an electrician and didn’t seem to be the typical low-HDL patient. The patient was interested in participating in the trial, and additional tests found his brother was also affected. “We were always adding one or two patients at a time, and it was always a very emotional experience,” notes Dasseux. “Tango is now a global study with patients in the U.S., Canada, Europe, and Israel.”
RELY ON LOGISTICS PARTNERS
Administering a protein-based biologic to patients spread across multiple countries and continents does complicate the logistics of a trial. To remedy the situation, an in-house team at Cerenis works with CROs to ensure the supply of medicines to patients is not interrupted.
“Having just 30 patients allows us to handle shipments on a case-by-case basis,” says Dasseux. “Much of the logistics effort is handled through CROs in the various countries, but in some cases our internal team is also involved.”
Getting patients to the clinic is an additional challenge. For example, the patients in Quebec are in the region of Chicoutimi, where the population is quite dispersed, and travel time to the clinic could take 2 to 6 hours. Clearly this is not an ideal situation, especially during the first two months when weekly IVs are mandated. In fact, some patients ended up not being able to participate in the trial because of the lengthy travel time. In some locations nurses traveled to the patient to administer the drug locally.
“This is an emerging technique, and it’s important to make sure everything is well validated,” explains Dasseux. “We need every patient to come to the clinic at the beginning of the study to have tests performed. If they cannot do that, they cannot participate in the study. We are doing our best to accommodate them. Although we do not pay the patients, we are also doing our best to make sure the trial is not costing patients anything out of pocket.”
KEEP EVERYONE IN THE LOOP
It’s very important to properly communicate with patients when running a rare-disease trial. In many cases, they do not know much about clinical trials and neither does their physician. For that reason, Cerenis has lengthy discussions with the treating physicians.
“These are general practitioners,” says Dasseux. “They do not have expertise in rare diseases or clinical trials, so we need to make them feel comfortable with the referral process. So, we discuss trials with them and have our internal experts, as well as independent industry experts, explain the process.”
Once the physician has a good understanding of the process, individuals from Cerenis will visit them to discuss the trial face-to-face. Later the CRO is brought into the process as well. The main goal of all these interactions is to preemptively identify potential challenges and discuss solutions. Dasseux stresses there are no one-size-fits-all activities when it comes to dealing with rare-disease physicians and patients.
Normally the physician visits will incorporate training such as good clinical practices. A video will explain how to properly prepare the IV solution. Refrigerators, water baths, and infusion pumps are required and are often provided by Cerenis to clinics that do not have the proper equipment on hand. Generally, the in-person visits take three days. If anyone is still uncomfortable with the process, a return visit is scheduled. A hotline is provided for sites to quickly connect with Cerenis or the CRO if there are questions.
“With any rare disease trial, we often have to go above and beyond what is typically required of a Phase 3 trial,” adds Dasseux. “We want to make sure every patient entering the trial understands if they do not complete the study, it could put the whole trial in danger. Each patient is a major contributor, and losing even one patient will have a big impact on the results.”
