The Netherlands — More Than Just The New Home Of The EMA

By Rob Wright, Chief Editor, Life Science Leader
Follow Me On Twitter @RfwrightLSL

In October I attended a press tour of the Netherlands’ biopharmaceutical industry. Sponsored by the Netherlands Foreign Investment Agency (NFIA), I imagine the impetus for the event was to tout Amsterdam being the new home (as of March 30, 2019) of the European Medicines Agency (EMA). While certainly a big deal, as the city and the Netherlands were selected from 16 locales vying for the opportunity, this was not what the tour was all about. In fact, the closest thing we got to see regarding the EMA was a happenstance drive by of the building under construction during the very last leg of the tour. And maybe that’s the point. For during the selection process, the EU assessed all host candidates on technical and softer requirements, including staff retention levels, with all three finalist cities (Amsterdam, Copenhagen, and Milan) anticipated to be able to keep at least 65 percent of current EMA staff post Brexit. So, what is it that seems to set this country’s biopharma sector apart? That’s what I hoped to find out.
Day One — Three Cities, Two Medical Centers, And Lots Of Startups
Erasmus Medical Center
The first full day of our tour began at the Erasmus Medical Center (Erasmus MC), which was described by Prof. Dr. Ernst Kuipers, chairman of the board of directors and CEO of the facility, as a “full merge between hospital, or as in our case, multiple hospitals, academic, tertiary care, research facilities, medical, nursing, and other schools.” Based in Rotterdam, it is affiliated with Erasmus University and home to its faculty of medicine, with the dean of the medical school actually sitting on the Erasmus MC board. With construction complete of its new building, opened this past May, it is the largest and most diverse of the eight university medical centers in the Netherlands. Employing over 17,000, Erasmus MC has an annual operating budget of €1.7 billion.
Kuipers gave us an overview of how the Dutch healthcare system differs from other areas such as the U.S. For example, in the Netherlands everybody has health insurance, and healthcare costs make up about 11 percent of GDP, which is 6.8 percent less than that of the U.S. Costing about €130/month/person, the annual out of pocket expenses (depending on the plan chosen) ranges from €350 to €850/year (max). Another difference involves how medical centers handle nonemergent patients. For example, in the U.S. just about anyone can show up at any ER and be given treatment. At Erasmus however, if a patient walks in seeking ER treatment, they are likely triaged by a family physician (FP) or a dentist, which they have on hand 24/7. This helps the facility weed out nonemergent patients, and thus why the Erasmus MC’s ER numbers (i.e., 45,000/year) are more comparable to that of a rural hospital in the U.S. Another difference is the number of hospital beds per inhabitant, which in the Netherlands is about 2.4 beds per 1,000 patients. “Countries like Germany and France have between 6.0 to above 8 hospital beds per 1,000,” Kuipers shares. “We can only work with such low numbers by being very efficient in flow between hospitals, between hospitals and home, primary care, and day care as much as possible.”
Following Kuipers overview of the facility and the Dutch healthcare system, we heard from a number of other experts, such as Prof. Dr. Casper van Eijck, a surgeon at Erasmus MC specializing in pancreatic cancer. According to Eijck, pancreatic cancer surgery is typically a six- to eight-hour operation, and something he believes will be obsolete in the near future. This is because pancreatic cancer tends to be very aggressive, and by the time it is typically detected it has already spread. Further, many patients following pancreatic cancer surgery often have recurrence, and long-term survival (i.e., ≥ 5 years) tends to be low (i.e., 5 to 15 percent). As a result, he and other pancreatic surgeons have become involved in large trials to see if adjuvant treatment could actually help patients. He pointed out how conducting research in the Netherlands can be very different that in other areas of the world, as the Dutch government encourages collaboration. For example, the PREOPANC-1 trial (a study where patients were randomly assigned to receive immediate surgery or chemoradiotherapy for 10 weeks, followed by surgery, with both groups also receiving chemotherapy post surgery), initiated in Germany and the U.S., failed to recruit enough patients. “By joining all of the university hospitals [in the Netherlands] together, we were able to finish this trial in three and a half years, with the preliminary data already having been presented at ASCO,” he noted.
But Eijck is looking for solutions to pancreatic cancer beyond surgery and chemotherapy. He then shared a story about two of his pancreatic cancer patients who seemed to be doing very well with a stable disease. “Every half year they’d come back, and were in really good shape,” he recalled. “So, after several years I asked them if they were doing anything else apart from previous treatments of chemotherapy.” As it turns out, both had been treating themselves every three to four months with an oncolytic virus, something he admits to having never heard of. “I went into the literature and found there were already a lot of publications on oncolytic viruses and learned how these attack tumor cells and enhance a patient’s immune system,” he stated. This led to the creation of a Netherland consortium to study if of oncolytic viruses could be used to treat pancreatic cancer. The research seemed promising, and Erasmus MC received a government grant, which is being used to buy the patent on the virus, and to build an oncolytic virus production facility toward improving pancreatic cancer patient care.
After hearing from Dr. Eijck, we took a brief tour of the hospital before being treated to some additional presentations. For example, we heard from Prof. Dr. Stefan Sleijfer, head of the department of medical oncology, who talked about the center for personalized cancer treatment (CPCT), a Dutch initiative between the Netherlands Cancer Institute-Antoni van Leeuwenhoek, Erasmus MC Cancer Institute and University Medical Center Utrecht (UMC Utrecht). Toward improving personalized cancer treatment, the center conducts a great deal of interesting research. For example, in a study conducted by Roelof W.F. van Leeuwen, it was demonstrated that drinking Coca Cola improved absorption of erlotinib (a lung cancer drug) in non–small cell lung cancer (NSCLC) patients. We met with Prof. Dr. Peter van der Spek, head of the department of bioinformatics, who illustrated how the medical center is using AI and 3D imaging to provide better patient care. We heard from Berry Kriesels, founder and CEO of Omnigen BV, a company using bioinformatics to reduce failures in clinical drug development. Finally, we heard Prof. Dr. Frank Grosveld, department of cell biology, who shared how when looking for novel types of reagents to be used in cells, they started to develop antibodies. Realizing the technology could be used for other therapeutic purposes, they worked with Erasmus MC to spin out a company, which is today known as Harbour Biomed, a global biopharmaceutical company developing innovative therapeutics in the field of immuno-oncology and inflammatory diseases.
Leiden Bio Science Park
Leaving Erasmus MC we headed north to the Leiden Bio Science Park (LBSP), home to Leiden University and Leiden University Medical Center (LUMC), several internationally acclaimed research institutes, and over 100 dedicated biomedical companies ranging from small startups to multinationals. The LBSP tour began with a working lunch at the Stal Grand Café. Now considered the clubhouse of LBSP, it was formerly where the company Pharming housed Herman, the first genetically modified bull whose offspring (cows) produced lactoferrin (an inflammation suppressant). Here we were treated to presentation by leaders of four innovative companies.
VarmX
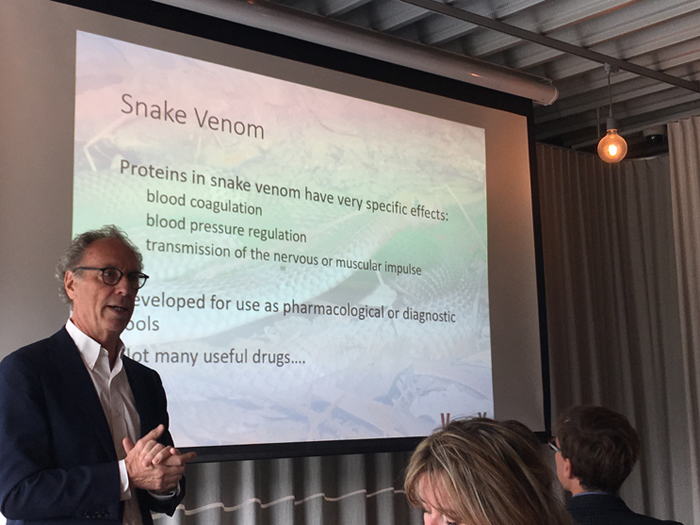
VarmX is a spin-off from LUMC, with a mission to develop and manufacture therapeutic proteins to restore hemostasis. Presenting on behalf of the company was its founder and chief scientific officer, Pieter Reitsma, a leading expert in the field of coagulation. “Every five minutes someone dies from a blood clot or deep vein thrombosis [DVT],” notes Reitsma. “In fact, one in every four deaths is caused by thrombosis.” To prevent we see increased use of new direct oral anticoagulants (DOACs), often indicated for ischaemic stroke in atrial fibrillation, venous thrombosis, pulmonary embolism, and prevention of DVTs following knee and hip replacement. The new standard drug for stroke and vein thrombosis is FXa (pronounced factor 10a) anticoagulant. Unfortunately, as helpful as FXa can be in treating patients, about 2 percent experience a side effect of a serious bleed, which can result in hemorrhage, hospitalization, transfusions, and if not successfully managed, death. “Where is the antidote to these anticoagulants?” he asks.
For inspiration, his company is turning to snakes, as proteins in snake venom have very specific effects, such as blood coagulation, blood pressure regulation, and transmission of the nervous or muscular impulse. For example, the eastern brown snake’s (Pseudonaja textilis) venom contains coagulation factor Va and factor Xa. A bite from one of these snakes is quite deadly, as a person experiences run away coagulation. But this gave Reitsma an idea. How might this snake respond to being given a popular oral anticoagulant? Turns out the snake is resistant. Could this insensitivity be identified and applied to human FXa? The short answer is yes, which led to the development of VarmX’s lead compound, PseudoXa, which has been shown to be a safe and effective reversal agent for prevention and treatment of bleeding in the presence of all FXa anticoagulants (class effect).
Fibriant
Fibriant is startup developing products based on recombinant human fibrinogen that initially targets hemostasis, host-defense and regenerative medicine applications. Presenting on behalf of the company was Jaap Koopman, the company’s founder and CEO. “Fibrinogen [a soluble protein present in blood plasma] is an extra ordinary protein,” he begins. “It is really big, actually twice the size of an antibody, and made of three polypeptide chains instead of two.” Koopman notes having been working as a biochemist on this particular protein for around 35 years. “What I love about fibrinogen is it is perfectly symmetrical, which isn’t the case with many proteins,” he grins. It is a very versatile molecule. For example, it can change its form from soluble, to insoluble, and back to soluble. “This is triggered by injury, which results in active thrombin,” he states. “Thrombin turns the soluble fibrinogen molecule into the insoluble fibrin polymer, which forms a network.” That network can be degraded again, as the lifespan of a fibrin network can be anywhere from a few hours to a few weeks. “It gets degraded by plasma into soluble fibrin degradation products.”
There are other reasons why Koopman is so excited about this protein. For starters, it plays an important role in four biological processes triggered by injury.
- Hemostasis (i.e., blood clotting)
- Tissue repair (following hemostasis)
- Inflammation
- Host defense against bacteria
But the most important reason is that fibrinogen is not one molecule. “In the blood of every healthy individual, it is a mixture of about 12 different variants that matter,” he explains. “Nowadays we [biopharma] make a lot of monoclonal antibodies, which is done by recombinant production. This is what Fibriant does for fibrinogen. We make monoclonal fibrinogen variants.” Koopman sees a variety of product applications, including surgery, tissue repair, inflammatory diseases and bacterial infections. The company’s current therapeutic product development activities are focused on fibrin as a flexible, biodegradable extra-vascular support matrix to prevent early and late state vein graft failure after bypass surgery. Koopman suggests that the market potential for products developed from fibrinogen could be comparable (if not greater) to the current market for monoclonal antibodies (i.e., $100 billion), providing for a bright future for his company.
Mimetas
Mimetas is the organ-on-a-chip company and has developed the OrganoPlate (a microfluidic 3D cell culture plate supporting up to 96 tissue models on a single plate). Paul Vulto, cofounder and comanaging director presented. “Mimetas is all about using this technology to provide human tissue and organ models to allow pharmaceutical companies to develop medicines of the 21st century,” he shares. “These same individualized models can be used to select the best possible therapy for individual patients, because that’s where things are heading with personalized medicine.”
The OrganoPlate looks like a microtiter plate, though the backside has been modified on microfluidics. “This product is fully compatible with any microscope equipment with robo handling,” he shares. Using PhaseGuides (a patented liquid handling technology), the OrganoPlate enables precise barrier free definition of culture matrices and cells in 3D, supporting cell-cell interactions and unprecedented imaging and quantification. Some of the applications for this technology include CNS toxicity studies and a range or neurodegenerative and psychiatric disorders. “We can grow human kidney tubules as well, which has applications in drug toxicity and kidney disease modeling,” Vulto notes. There are other applications, which biopharma companies seem to have found valuable, as Mimetas is already working with 30 of the top 50 pharms in the world.
Ncardia
Ncardia is a stem cell drug discovery and development company currently operating worldwide. Stefan Braam, CEO, conducted the presentation for the company that was formed through the 2017 merger of Pluriomics (founded in 2011) and Axiogenesis (founded in 2001). “We start with humans, and we use Nobel Prize iPS cell [induced Pluripotent Stem Cell] technology,” he shares. “Our core expertise is assay development, and our goal is to be the trusted partner for scientists operating in the hiPSC [human induced Pluripotent Stem Cell] drug discovery and development space including cardiovascular and neural safety and efficacy studies.” Braam then provided an overview of the company’s products, services, and global operations.
Leiden University Medical Center
After the working lunch, we walked over to the Leiden University Medical Center (LUMC) for a presentation by Dr. Ton Rabelink, professor of nephrology. Now for those unfamiliar with Leiden University, it was founded in 1575, and is home to 16 Nobel Prize winners (either former students and/or faculty). “In this hospital,” Rabelink begins, “Regenerative medicine, together with oncology, has been prioritized as one of the main areas to do research.” The reason for the prioritization of regenerative medicine is based on the fact that the Netherlands is relatively small (i.e., 17 million inhabitants), yet spends roughly €18 billion/year on a few chronic conditions (e.g., heart disease, diabetes, kidney failure). Further, about four years ago the Dutch government made a public inquiry to the general population on where they thought the government should invest resources in scientific exploration. “Regenerative medicine was one of the priorities expressed by the Netherland population,” he notes. Dr. Rabelink went on to explain how several initiatives at LUMC, such as the Leiden stem cell and vector facility and iPSC nursery come together to form the regenerative medicine network, which ties into the EU’s Horizon 2020 program.
We were then given a tour of an LUMC lab by Marten Engelse, head of the laboratory for regenerative medicine and pancreatic islet isolation. During the tour I was extremely impressed with Engelse’s ability to teach with great enthusiasm. “What I want to impress upon you is that organ transplantation is basically a form of cell therapy, if you start looking at it from a production point of view, which is cells in a matrix with blood vessels,” he explained. Engelse went on to discuss his current area of focus around kidneys and the self-organizing capacity of cells.
We concluded our time in Leiden with a visit to Janssen Vaccines, where we were provided a presentation by Hanneke Schuitemaker, head of viral vaccine discovery & translational medicine, and Dirk Redlich, head of vaccines process & analytical development. Our first day of the press tour concluded with a networking dinner in the city of Nijmegen, where we were greeted by the city’s mayor, along with folks and executives involved in the local area’s life science/biopharma sector.
Stay tuned for experiences from Day Two of the Netherlands’ press tour.
