What Drives Better Public Health Policies And Superior Patient Outcomes
By Suresh Kumar
 Obsession with repealing the ACA without a coherent alternative or goal and the scourge of Ebola striking yet again in the Congo lead me to conclude that policy makers and industry leaders need to be more grounded on the purpose of their endeavors. They must articulate national and global aspirations and how industry can profitably and sustainably support the common good. Agreeing on the what is a prerequisite for not disagreeing on the how while determining the pathways to pursue. These steps also help address waste, fraud, and abuse to immediately contain costs.
Obsession with repealing the ACA without a coherent alternative or goal and the scourge of Ebola striking yet again in the Congo lead me to conclude that policy makers and industry leaders need to be more grounded on the purpose of their endeavors. They must articulate national and global aspirations and how industry can profitably and sustainably support the common good. Agreeing on the what is a prerequisite for not disagreeing on the how while determining the pathways to pursue. These steps also help address waste, fraud, and abuse to immediately contain costs.
U.S. PUBLIC POLICY 101: PLACING BETS TO IMPROVE OUTCOMES AND BEND THE TRAJECTORY OF COSTS
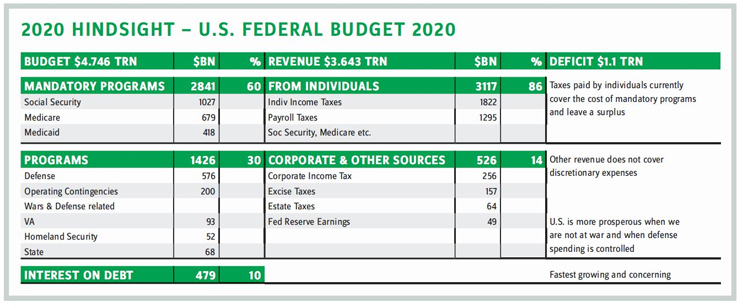
Understanding why, where, and how government spends monies helps frame what society seeks, how it pays for what it seeks, and its ability to hold government and industry accountable for what it seeks. Understanding these factors also helps show how public health fits within a broad framework of national policy (See table: 2020 Hindsight — U.S. Federal Budget 2020). Here are a few truisms:
- Individuals’ taxes contribute $3.1 trillion i.e., 86 percent of revenue collected.
- Mandatory spending of $2.8 trillion on programs directly benefiting individuals including healthcare is capped at 60 percent of budget.
- Discretionary spending ($1.4 trillion, 30 percent of the budget) is overwhelmingly for defense and war efforts. Indexing this spending to a measure of revenue generated from sources beyond income and payroll taxes is fiscal prudence.
- The annual budget deficit of $1.1 trillion is not sustainable; interest on debt is the fastest growing item after defense spending.
- U.S. prosperity is greatest, and population health is at its best (lower incidences of disability, PTSD, etc.), when we are not engaged in wars.
- U.S. public spending on healthcare is consistent with that of advanced and wealthy countries. U.S. private healthcare spending (insurance premiums, deductibles, copays, out-of-pocket costs, liability for undecipherable hospital charges, etc.) is over three times that of other comparable countries.
- The U.S. is characterized by fewer physician consultations per capita, shorter hospital stays, higher cost of procedures, greater installed capacities that increase cost (e.g., of imaging and MRI), and significantly higher cost of medicines. For example, compared to the U.K., Xarelto is more than double the price, and Humira costs 96 percent more in the U.S. The difference between gross and net prices obfuscate; discounts neither explain value or make a material difference.
- A larger population living longer predicates higher healthcare spending every year, but capping spending per capita or as a percent of GDP is fiscally prudent policy.
Our policies abandon affordable alternatives of prevention and preemption. For example, funding diplomacy and international development will reduce or prevent conflicts, decrease the loss of American lives, and reduce tragic health-related costs of war. In some of my past columns I’ve explained the real and current danger of not prioritizing and promoting prevention in our healthcare policy. Caring for a growing population — and one with an increasing incidence of chronic disease — via a medication-in-perpetuity model is myopic; it will neither improve health nor bend the cost curve.
What should our healthcare policy accomplish? Should it:
- ensure everyone has access to health insurance and physical and mental healthcare?
- reduce absolute incidence of defined chronic diseases and as a percent of the population?
- reduce incidence of behavioral health-related mortality (substance abuse, drug overdose, suicides, gun related deaths)?
- increase well-being as measured by percentage reductions in:
- incidence of obesity?
- food and beverages with sugar and salt above threshold levels?
- mandate that school children be educated in healthy living, nourishment, and behaviors?
Aligning programs and priorities is impossible without clarity of purpose.
PROTECTING THE VULNERABLE AND INSULATING ALL FROM INFECTION
Ebola first struck in 1976 in the Congo. Over the years, the disease has spread, with cases being detected in the U.S. and the U.K. Consequently, there has been increased public focus on the global risk of the disease and the flawed readiness and response protocols to combat infectious disease in general.
Today, we are far from preventing, detecting, containing, and eliminating the disease. Consensus between donor and recipient nations regarding the purpose of global public health policy remains as elusive as efforts to objectively measure progress. Defining the shape, cost, and funding of interventions, and which innovations will be pursued, is daunting but addressable.
Although it’s necessary to create conflict-resolution initiatives and build roads, power grids, cell towers, and hospitals in large urban centers, all of these tasks are outside the remit of global public health. These must be the responsibility of local governments and international and aid-giving institutions. What must global health policy accomplish for donor or recipient governments, the WHO, or other UN and UN-like agencies, and for civil society? Some suggestions include:
- assistance developing robust health systems, help with training health workers, paramedics, and epidemiologists for rapid deployment in Africa
- affordable vaccines and medicines for vulnerable communities, funds for stockpiling if necessary, and pricing indexed to the robustness of inoculation, public health, and hygiene education programs in a country
- innovations such as cheap, modular, rapidly installable prefab clinics with electric generators and a water supply that all can be incinerated if infected
- technology such as drones to drop critical medical supplies or collect blood samples for rapid analysis
- telemedicine services that connect global infectious disease specialists with local medical professionals to mitigate the shortage of doctors and rapidly combat disease.
THE WAY FORWARD
Thanks for the many comments on my last column. Reader Tom Haling asked, “When free markets do not deliver the great solutions that they generally do, what is the role of public policy? Solving the problem? Changing the incentives to the free market? The system and companies are focused on ’tending to the sick’; pharma annual reports have a profitability focus. We need to improve our education system. We need to include wellness in the curriculum.”
I stated in my inaugural column, “I will share my perspective, raise questions, and paint a picture of the emerging future.” My goal is to provoke thinking and enroll more of us to help build better public health policy. We are well on our way on that journey.
SURESH KUMAR serves on the board of Jubilant Pharmaceuticals and Medocity. Formerly, he was U.S. Assistant Secretary of Commerce and Executive VP at Sanofi.
