What Is Necessary To Keep Populations Safe
By Suresh Kumar
 By Feb. 24, COVID-19 had infected 79,400 people and claimed 2,600 lives across 30 countries. An epidemic, it threatens to become a pandemic. China bears the brunt of infections and fatalities, but novo-coronavirus is a stark reminder of global connectedness. Travel and commerce can be impacted by nationalistic policies and trade wars; however, disease and illness cross borders with impunity. Has the global community performed well to contain the spread of disease or fortuitously dodged a bullet?
By Feb. 24, COVID-19 had infected 79,400 people and claimed 2,600 lives across 30 countries. An epidemic, it threatens to become a pandemic. China bears the brunt of infections and fatalities, but novo-coronavirus is a stark reminder of global connectedness. Travel and commerce can be impacted by nationalistic policies and trade wars; however, disease and illness cross borders with impunity. Has the global community performed well to contain the spread of disease or fortuitously dodged a bullet?
EPIDEMICS: A RETROSPECTIVE
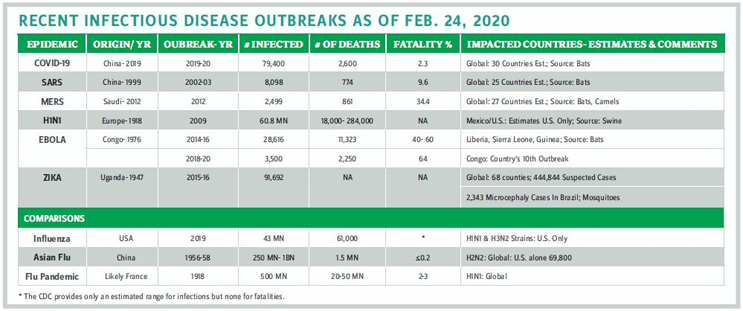
The young 21st century has already witnessed more frequent infectious outbreaks of epidemic proportions (see table) than in the past. The latest, COVID-19, has locked down a metropolis of 11 million people and caused widespread disruption to life and work across China. Outbreaks in urban areas are ominously riskier; insulating high-population centers from rapid infection-causing pathogens is an urgent urban planning and public health necessity. International travel and the increasing urban sprawl from metropolis to megapolis create a risk that cannot be ignored. The conundrum remains: Outbreaks start locally, so how can a response be mobilized globally?
CANDOR MOBILIZES PUBLIC TRUST AND GLOBAL SUPPORT
Epidemiologists have made progress on tracing and quantifying the trajectory of infections, but trust in data and its timely sharing remain elusive. COVID-19 was likely first established in December 2019. By Christmas, doctors reported cases of it spreading among medical workers. Yet, the genetic makeup of the virus was not shared in public databases until Jan. 11. Protocol for identifying, isolating, and treating patients and contact tracing were not established until Jan. 23. Porous borders resulted in cases of COVID-19 outside China (e.g., Thailand reported one on Jan. 13). Yet, this is an improvement over SARS, when China took three months to acknowledge the infectious breakout and over four and a half months to share details globally.
Listen and speak to the world. Early sharing and openness to allow global expert teams on the ground helps accelerate intervention and containment. Sharing information and seeking expert assistance does not stigmatize countries; it protects populations. How can intervention protocols be established globally, and more importantly, enforced locally across sovereign nations? Epidemics are not just one country’s problem; they imperil the world.
Listen and speak to medics on the ground. The trajectory of COVID-19 could have been different had local health agencies listened to the suspicions of ophthalmologist Li Wenliang that led him to alert colleagues of a potential outbreak. In contrast, the world owes a debt to Nigerian Dr. Stella Ameyo Adadevoh, who in July 2014 diagnosed and isolated a Liberian later identified as Ebola “patient zero” in Lagos. That action preempted devastation in the densely populated 20-million-people megapolis.
Building trust in public institutions, gaining agreement on deploying global protocols, and developing funding mechanisms are the foundations of sound global public health policies. The long list of learning to combat and preempt epidemics includes:
- early, frequent, and robust communications with the public and with the scientific community
- rapid response management
- development protocols for diagnostics, treatment regimens, and vaccines and medicines
- strengthening public health infrastructure and programs
- public education on hygiene, diet, customs, and conventions
- developing institutional capacity building
- training cadres of healthcare workers who can be deployed in emergencies.
FRAMEWORKS OF GLOBAL ENGAGEMENT FACILITATE GLOBAL PUBLIC HEALTH INTERVENTIONS
As a response to the worst Ebola outbreak, the WHO’s R&D Blueprint was born at the World Health Assembly in May 2016 to establish a global strategy and preparedness plan. It includes:
- global coordination mechanisms, funding, and communication protocols
- accelerated R&D: prioritizing disease, road map and target product profiles, regulatory and ethical pathways
- developing norms and standards: clinical trial designs and data and sample sharing
- response planning including, in the event of an outbreak, mechanisms to shift the focus of the blueprint from R&D preparedness activities to an emergency R&D response plan.
The R&D Blueprint acknowledges the need to plan for the unknown. Combating unknown pathogens by enabling crosscutting R&D preparedness across identified diseases to combat “Disease X” is a major, if linear, step to rapidly confront the spread of infectious disease.
The National Institute for Allergy and Infectious Diseases (NIAID) at the NIH used research investments post SARS and Middle East Respiratory Syndrome (MERS) to develop diagnostics, therapeutics, and vaccines against coronaviruses. Within two weeks of the discovery of COVID-19, researchers determined how it enters cells and are adapting platforms to develop diagnostic tests and vaccines while also evaluating broad-spectrum antivirals and potentially monoclonal antibodies treatments.
LEVERAGING SCIENCE & TECHNOLOGY FOR CREATIVE SOLUTIONS
Scientists from Australia’s Commonwealth Scientific and Industrial Research Organisation (CSIRO), Alphabet’s Verily, and the James Cook University leveraged technology to scale sterile insect techniques in a bid to eliminate Zika and mosquito-borne disease. This required breeding enough Aedes aegypti mosquitoes to suppress a population, removing biting females, identifying the males, and then releasing millions of sterilized nonbiting males to mate with local female mosquitoes across the Queensland’s Cassowary Coast. This resulted in eggs that did not hatch and a significant reduction of their population between November 2017 and June 2018. Can similar science be applied to neuter disease-carrying bats that are the root cause of several infections?
Operationally, China segmented patients by intensity of infection to optimize resources and assign patients between hospitals and nursing homes, while successfully setting up 1,000-bed prefab hospitals that could serve as a template for the future. Similarly, sealed prefab clinics complete with critical commodities — electric generator sets, water, and medical supplies — can help care for and isolate Ebola patients. Infections can be contained, if required, by incinerating these lower-cost infrastructures.
BUILDING COALITIONS TO STREAMLINE INSTITUTIONS AND ENLIST ALL STAKEHOLDERS
Creative solutions can preempt disease, and smart interventions such as tents and rehab structures come at lower costs than permanent buildings. Every line item of current global public health costs must withstand scrutiny. Institutional responsibilities need streamlining with some focusing on science, others on epidemiology, and yet others on operations to train boots on the ground. I have advocated for this over the years from the World Economic Forum in Davos, to the World Health Summit in Berlin, and at the Organisation for Economic Co-operation and Development (OECD) in Paris. Public institutions must lead responsibly, the private sector must be enlisted to develop and deliver solutions, and nations must strengthen public health initiatives (e.g., link aid and product pricing to the robustness of vaccination programs). Capital markets and society must be tapped to sustainably fund interventions.
Keeping populations safe is not a proxy for incremental cost nor an investment tradeoff between infectious and chronic disease. COVID-19 is a stark reminder: Complacency toward global public health is not an option.
SURESH KUMAR serves on the board of Jubilant Pharmaceuticals and Medocity. Formerly, he was U.S. assistant secretary of Commerce and executive VP at Sanofi.
