Codagenix: A Tiny Start-Up Ready To Take On The Goliaths Of The Vaccine Industry
By Wayne Koberstein, Executive Editor, Life Science Leader
Follow Me On Twitter @WayneKoberstein
The Enterprisers: Life Science Leadership In Action
One egg per person. That is what it takes to produce a flu vaccine. The standard, predominant method has not changed in more than 70 years. What has changed dramatically, however, is the per-unit cost of goods, price, and scarcity of the product; all have risen steadily, to the point now where the old model of universal vaccination seems more antiquated than the aforementioned egg. Arguably, newer, recombinant and cell-based production technologies have only compounded the cost/supply dilemma for vaccines, without a commensurate rise in mass efficacy. What if a company had a technology that could sharply lower CoG (cost of goods) and ensure the highest possible availability and effectiveness of an influenza vaccine — even though the company were a David up against the flu-shot Goliaths?
 Codagenix believes it is that company. Starting with flu, then moving on to other disease vaccinations, the tiny start-up wants to turn the entire field of action around.
Codagenix believes it is that company. Starting with flu, then moving on to other disease vaccinations, the tiny start-up wants to turn the entire field of action around.
A MARKET ADRIFT
It had been a long day, and the late-evening reception was dying down. I found a couch in a side area where my tired old bones could rest. Soon others joined me on the couch and nearby chairs, and I struck up a conversation with the person next to me, who turned out to be Steffen Mueller, cofounder, president, and chief scientific officer of Codagenix. Beside him was COO and cofounder J. Robert Coleman.
Yet, even before Mueller and I exchanged cards, we had already dived into a discussion about vaccines. Unlike most of the people around us at the time, I was alive during the great polio epidemic following World War II. I lost my older brother to the disease in 1950, later tagged along with my mother each year in the March of Dimes, and lined up with just about every other kid in the country for the first vaccine. But I was struck by how close Mueller’s views of the situation were to mine. We both expressed dismay at the drift of vaccination from a universal, public-health-driven enterprise, to a fragmented and fractious, albeit high-profit endeavor. Unlike me, however, Mueller and his company may have a solution — not just another way to make more vaccines, but a way to make them better, by many thousands-fold.
Months later, I followed up on our chance meeting in a longer talk with Mueller and Coleman for this article. The story of their little company carries a large meaning. Any real challenge to the status quo of vaccines could only come from an obscure entity such as Codagenix. From a business standpoint, scant motivation for change exists; vaccines have become highly profitable for large companies almost in direct inverse proportion to the drop in their universality. When everything is so cozy for the establishment, the desire to shake things up may grow stronger in the outside player.
Other vaccine start-ups have also entered the field lately, such as the mucosal vaccine company Mucosis, covered recently in Companies to Watch, which only reinforces the medical need for new approaches in the space. Codagenix makes a good choice for The Enterprisers because its audacious mission, set against the high risk of development still at the preclinical stage, signifies not only a potential vaccination breakthrough, but also a significant entry into synthetic biology. Its technology is meant to replace the age-old trial-and-error method of vaccine creation by configuring the entire genetic makeup of the live attenuated virus to be mass produced. So rather than competing with other new approaches, it may actually be complementary or compatible with them.
VIRAL TAMING
Codagenix counts on its Synthetic Attenuated Virus Engineering (SAVE) platform to transform vaccine creation into an exact science. SAVE is proprietary software for configuring live vaccines made of viruses that match the wild types in every respect except one: their ability to cause disease. With SAVE, the company synthesizes the whole genome of a virus, but with strategic changes in certain codon pairs to “de-optimize” the mechanism supporting its virulence.
The technology emerged from research headed by Eckard Wimmer at Stony Brook University. Wimmer made history, and stirred some controversy, by synthesizing the polio virus for the first time in 2002. SAVE has passed proof-of-concept studies in animals successfully and will soon face its next big test in human trials. Like so many of the novo-vaccine companies, but perhaps with stronger logic to support it, Codagenix has chosen flu as its lead vaccine target. In keeping with SAVE’s broad potential, however, the company also has pipeline programs for respiratory syncytial virus (RSV), Dengue Fever, foot and mouth disease virus (FMDV), pathogenic E. Coli, and other diseases.
“We are developing our approach to dramatically impact global health by making designer vaccines that are genetically stable, safe, and effective. That is the central core of the company,” says Coleman. “Our platform is a software-based approach, a genome-design technology. It is a platform because theoretically we could apply it universally, to any virus.”
The term “platform” does apply to SAVE, but in an unusual sense — the platform consists of bytes, not material bits. SAVE is also unusual in what it produces at the end: an entire genome rather than the virus-like particle or backbone virus with a few antigens attached in current vaccines. The SAVE-modified genome is synthesized in its DNA form and recovered by recombinant DNA technology in appropriate tissue culture cells. Uniquely, SAVE faithfully reproduces the wild-type virus for a vaccine, but de-optimizes codon pairs in the viral genome involved in causing the host cell to produce proteins for the virus. The de-optimization slows down the protein production to the point that, when the vaccine activates an immune response, it also buys time for the immune system to overwhelm the virus before it can adapt and escape.

"When we started trying to raise private money for our clinical work, we met with a lot of resistance."
J. Robert Coleman
So what is “de-optimization?” My take on the concept: Codon pairs are redundant genes that reinforce each other’s activity. If you exchange a key proteinencoding codon for a similar but less active codon copied from elsewhere in the viral genome, it will still stimulate protein production but at a much lower rate. Although the host’s immune system sees the reengineered virus in the vaccine as identical to the wild type in the proteins it engenders, the vaccine virus lacks the wild-type ability to coax host cells into producing those proteins fast enough for the virus to outrun the immune response and survive. The deoptimized virus dies off, leaving the host immunized against the wild type as would a traditional weakened-viral vaccine — but potentially with much greater efficiency.
“Forever in the vaccine industry, companies have always tried to make more antigen, but our approach is actually to lower the level of translation of the virus,” Coleman says. “Wild-type viruses use codons and codon pairs that the human host cell reads quickly. We use exactly the same amino-acid sequence as the wild type, so our vaccines are a perfect match to the target at the protein level. But we encode those proteins using codons the human host cell reads much more slowly.”
Mueller explains what the de-optimization MoA (mechanism of action) means to the end product: “The vaccine virus presenting to the immune system is a 100-percent identical replica of the real thing, so the immune response should be the best possible match, which seems to be the reason our vaccines can be effective at an extremely low dose. The effective dose appears to be orders of magnitude lower than any other vaccine approach we’ve seen or read about in the literature, and it could be a real game changer.”
BUILDING EXPECTATIONS
The Stony Brook research team headed by Wimmer began work on SAVE around 2004, eventually yielding several papers, including two strong studies published in 2010 — one in Science on the possible applications of synthetic viruses, the other in Nature Biotechnology on using a computer-designed synthetic virus as a flu vaccine. Then they waited for thunder on the horizon. Alas, they waited in vain.
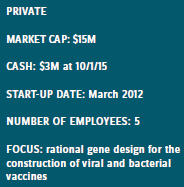
“Because our technology is so cool, we always hoped the Big Pharma companies would just run to us and break down our doors. But nobody came knocking,” Mueller recalls. Mueller, then an assistant professor, and Coleman, a graduate student, were both on Wimmer’s team and were determined to carry the flag forward. Coleman left to complete his postdoc at Albert Einstein and his MBA at New York Institute of Technology, but Mueller had already incorporated the company during a Stony Brook business workshop in 2009, though he had since come up empty in repeated applications for SBIR (Small Business Innovation Research) start-up grant money from the NIH. After Coleman returned in 2011, however, the two reapplied for an STTR (Small Business Technology Transfer) grant with Dr. Wimmer, and this time were successful. They booted up the company and moved into its current laboratory at the Long Island High Technology Incubator (LIHTI), adjacent to the Stony Brook campus. Since then, the company has lived mostly on additional grants, though it finally closed on its first VC investment this year.
Both Coleman and Mueller acknowledge the quest for venture and other equity funding has turned out to be more hardgoing than they once expected — in fact, their biggest hurdle so far. They have developed a more seasoned view now, coming to see vaccines in general, and their company’s approach in particular, as appropriate only for a special kind of investor.
“It takes someone with a long-term view of investment and perhaps being a bit more philanthropic than profit-driven,” says Mueller. “I am sure many investors prefer something with a higher profit margin than vaccines.”
Coleman adds that investors in vaccines naturally have a longer time horizon, which limits the potential VC and partner pool for Codagenix. “Vaccine investors must also have some interest in global health, because vaccines will never be a product for which you can charge prices that make it extraordinarily profitable at the individual unit level,” he says.
“Obviously, if you have a successful vaccine, you will sell a lot, and that could be profitable, but the time from bench to market for vaccines is probably the longest of any medicine. There are also a lot of other early vaccine developers with essentially me-too technologies, and the lack of novelty has cooled investment in the space as well. We finally found some investors who had a yen for the long-term horizon and saw our flu vaccine as not just another me-too, but as a potentially disruptive technology.”

"Because our technology is so cool, we always hoped the Big Pharma companies would just run to us and break down our doors. But nobody came knocking."
Steffen Mueller
CHASING GOLIATH
Codagenix has one thing in common with other new vaccine companies, however — its choice of influenza as the target of its lead program. Many analysts, reporters, and investors have wondered aloud why every young David in the business wants to take on Goliath. But Mueller and Coleman believe targeting flu is the most definitive way to demonstrate the economies of scale afforded by a SAVE-produced vaccine.
“When we started trying to raise private money for our clinical work, we met with a lot of resistance,” says Coleman. “Investors would say, ‘Why would you want to make a flu vaccine? There is already one that makes $4 billion or more a year! So unless you have one that is really fantastic, don’t even bother.’ But that is what we are trying to do — make a disruptive vaccine. The current standard flu vaccines have very low efficacy, especially year to year. For example, last year’s H3N2 component of the current vaccine had only about a 9 percent efficacy rate. We still tell people to get their flu shots, because even a poor vaccine can produce some herd immunity. And they are profitable. But our flu vaccine may achieve universal efficacy at a greatly reduced cost of goods.”
Coleman argues that growing vaccine virus in eggs makes them inherently less immunogenic, and at best, he says, current flu vaccines offer only a 25-percent match to the strains specified by the WHO each year, by matching only two of the eight major influenza virus proteins. “Our platform is capable of providing a vaccine with a 100-percent match; thus we hypothesize it may have greater efficacy than the current flu shot — and that fits the definition of a disruptive technology.”
Through the rough times of chasing private equity, the company kept its concept alive mainly with the help of the U.S. government. SBIR and the USDA repeatedly came to the company’s aid with money to finance its next needed steps. But Coleman has one suggestion for improvement in the programs.
“The granting agencies should place more emphasis on the earliest of stages in vaccine development,” he says. “It is the hardest step for a vaccine company. For other drugs, maybe the Valley of Death is Phase 1 to Phase 2, but for a vaccine company, it comes at an earlier stage, even before getting into the clinic. That is hard because there is a lot more government support for vaccines after you get through proof-of-concept.”
Undoubtedly, new vaccines and other high-potential technologies experience some of their toughest tests at their earliest stages, as do the companies that champion them. Perhaps, too, the more radical the changes to be wrought by those technologies, the more critical is early financial support to their success. Rather than “kill early” in such cases, maybe the operative principle should be “nurture early” to prove or disprove the concept. Not only could such a practice winnow the chaff from the wheat among development candidates, it might also ensure the surviving candidates enter clinical trials with the strongest possible data to support them. Codagenix appears confident its preclinical work has laid a long, wide, and breakthrough path for its synthetic-virus vaccines.
VACCINES: CHANGING A CHANGED WORLD
A new biography of Dr. Jonas Salk, inventor of the fi rst killed-virus polio vaccine in the 1950s, describes how the entire U.S. society mobilized to fi nd a cure or prevention for the disease. Housewives joined the March of Dimes by the millions to educate their communities, collect donations, and even gather patient data for clinical trials. They also made sure all children lined up to receive their vaccinations. The question is, could such a united public health effort happen again, for prevention of diseases that threaten us all? Steffen Mueller, president and CSO of Codagenix, answers:
"I believe not, because in today’s Western society, people are no longer confronted as much with infectious diseases, and polio is a prime example. It was very visible in the 1950s. When someone had polio, everyone saw it, and it was scary as hell. But such fear of infectious diseases is now gone, and instead we have all the vaccine deniers trying to poison the well, and unfortunately a lot of people listen to that. With the first polio vaccine, the risk-benefit calculation back then was made at the highest level. Now it’s an individual risk-benefit analysis, and that’s dangerous, because it leaves it to the individual to decide, ‘Do I want to vaccinate or don’t I?’ Many people now say, ‘I don’t see these diseases, so I’d rather not vaccinate myself.’ Eventually, it will swing back to where too many people choose not to vaccinate, and then, boom, all the old infectious diseases will come roaring back. I’m afraid that is what it will take for the population to wake up and say, ‘Why are there no vaccines? Where is the vaccine for this disease?’"
